Last year I wrote a top 10 list of the important stories of my life for the year 2016. It was a very eventful year and it really didn’t take much effort to come up with 10 different things to occupy my list.
In some respects is been a less eventful year in that there have not been 10 big topics. That doesn’t mean it has been uneventful. This year the big news items have been more broad themes rather than distinct issues or events. Also in some ways it seems that did not happen are almost as newsworthy as the things that did happen.
Rather than make an enumerated top 10 list like I have done in some previous years, I’m just going to talk about the big themes of my life without trying to arbitrarily divide them into 10 individual events.
Adjusting to Life With a Trach
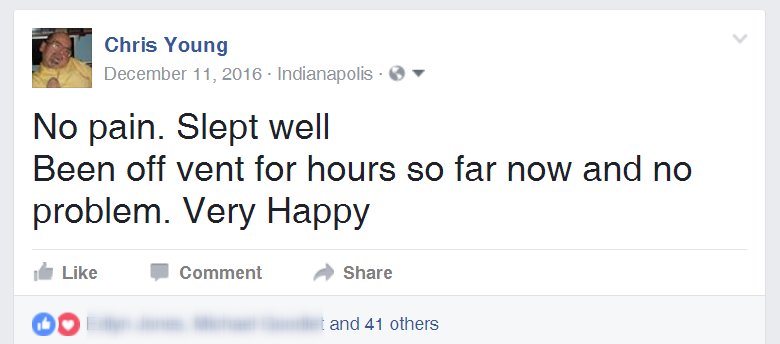
I came home from the hospital from my respiratory problems and the installation of my new trach on December 28, 2016. The consequences of having new trach affected nearly every part of my life for this past year. Some of it was directly related to the trach and other items were sort of a side effect of the uncertainty of my health on a day-to-day basis.
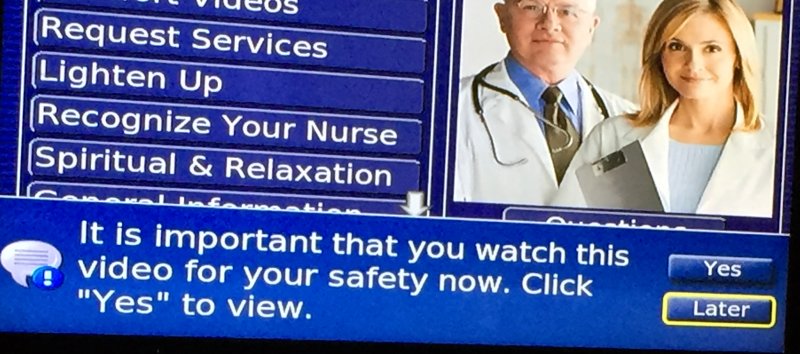
Having a trach meant that I was no longer using a CPAP but instead used a ventilator. Like the CPAP, I only used the ventilator at night. There was quite an adjustment learning how to manage the trach, getting a routine for getting me off and on the ventilator each day and coming up with ways to communicate while I was on the trach and could not talk.
I have the ability to use my laptop connected to my bedroom TV by just pressing three buttons. I set up a system of ready-made messages in the form of off-line static webpages that I could click on using the buttons as a mouse control. These messages gave dad step-by-step instructions on how to get me off the ventilator. Of course after a month or so it had become so routine he could just come into my room in the morning and say “Are you ready to get off” and I would wiggle my eyebrows up and down which is my way of saying “Yes” and he would go from there.
Windows 10 also has a built in on-screen keyboard that does a primitive single switch scanning method that allows me to type anything I want. Unfortunately it is only single switch, not dual switch, which makes typing extremely slow and inefficient. It does have a word prediction capability but it is not nearly as sophisticated as what is available on my iPhone or iPad under iOS. I’m still using it to type messages when necessary.
Over the first few months my routine was that I would wake up in the early hours of the morning say about 4 – 5 AM and could not get back to sleep. I would need to roll over on my right side to get comfortable. That meant we had to temporarily take me off of the vent, put in the speaking valve so I could talk, roll me over and I would be able to tell dad what I needed in the way of adjustments, and then put me back on the vent.
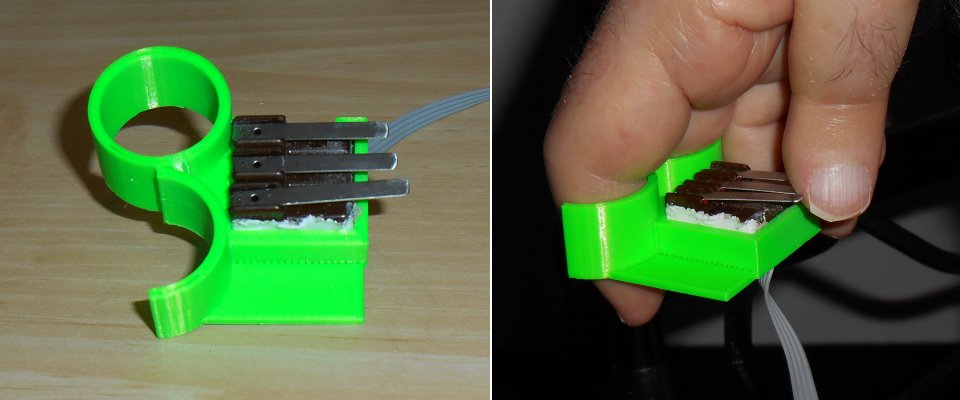
Once lying on my side I could no longer see my TV screen connected to the laptop so I could not type messages. So I purchased an iPad 2 mini and propped it up using a 3D print stand. Here’s a blog post about the new iPad and how I use it.
However in recent months I’ve been able to sleep reasonably well until about 8 AM when dad wakes up. So I’ve not been turning over on my side and have not needed the iPad as much as I did early in the year. It’s still available if I need it. If I ever end up in the hospital again, it will be an important part of my communication system.
Early in the year right after getting out of the hospital, I didn’t really have the stamina to stay up out of bed as much as usual. If I went to bed early, it often meant that I had to skip one of my G-tube feedings because it’s dangerous to do a feeding while lying down flat. So we quickly decided that it was time to get me a hospital bed. This will allow me to take a feeding while in bed and to partially elevate for at least 30 minutes after the feeding to avoid possible reflux and aspiration. The ability to partially sit up in bed was also more comfortable when using the bedpan for bowel movements. Of course there was the usual difficulty of getting insurance approval and getting the vendor to return phone calls, fax forms, etc. but we eventually got the new bed and it’s working out well.
Nursing and Home Health Aids
When I first got my G-tube in May 2016 it meant that my home health aide could no longer feed me my lunch. Although the process of doing a G-tube feeding is pretty simple, the rules say that a CNA aide is not allowed to deal with a G-tube. Now that I have a trach, the restrictions are even tighter on what a CNA can do. Most notably they are not allowed to be alone with me in case my trach needs suctioning. Dad typically would do his grocery shopping on Tuesdays while the aide was here getting me dressed. He would also schedule doctor’s appointments during the morning when they were here. Or occasionally if the aide was free we would get them additional hours to stay with me in the afternoon.
Although all of my case management people insisted that they would be able to get me nursing hours to take care of these kinds of situations, it didn’t happen until late in the year. Initially we had some nurses doing visits twice a week just to check up on me and see how I was doing with the new trach. They were able to resolve some issues with the pharmacy where I could not get nebulizer medicine. But other than that, these biweekly visits didn’t do much. These nurses were only able to do brief visits and were not in the business of staying with me for any reasonable amount of time while dad would go out. We needed a different agency for that.
It wasn’t a problem of getting authorization. The problem was finding an agency that could staff the position. Apparently it’s easier to get a nurse for eight hours a day on a regular basis then it is to get one for a couple of hours a week like we needed. At one point we thought we had nursing assistance lined up. However it turned out they were going to try to send ordinary CNA people even though that was against the rules. That plan got rejected by Medicaid and I don’t know if it was my case or a collection of cases for which that agency eventually lost its accreditation.
Dad had a variety of health issues which we will discuss in a later section. This meant that in addition to his normal doctor’s appointments he had lots of other appointments and procedures. That meant that either Carol had to take time off work or that our friends the Byrams or Brakes had to stay with me.
The aide that I had before I went to the hospital was a nice gal named Riah. In my absence she had rescheduled other clients and was not able to work for me every day. Initially she split days with another girl named Brooke. Brooke eventually got tied up with nursing school and after just a few weeks I had Riah back full-time. Additionally we got authorized for seven days a week where previously we had only been able to get six days a week.
Riah is a hard worker and a good friend but her life is very complicated. She is a single mom of six kids. One of them has ADHD and so has had numerous issues at school. Her three-year-old has severe respiratory problems which has had him in and out of Riley Children’s Hospital on many occasions. He is currently in Riley awaiting a lung transplant. All of the above plus car repairs has meant that she has missed a lot of work. It’s not practical to train another aide as a backup so many occasions we’ve had to do without help. However when she is here, she does such a good job and we get along so well that it’s worth dealing with her absences.
Eventually we were able to find an agency that could supply a nurse for a few hours a week so dad can run errands and go to the doctor. We are authorized for 15 hours per month. If we use two hours per week for dad to do his regular grocery shopping, that leaves us about seven hours per month for doctor’s appointments and other activities. We were assigned a nice guy named Mohammed. We get along really well. He’s fascinated by a variety of religions in addition to his own faith of Islam. We get into lots of friendly religious discussions mostly me explaining various parts of Christianity to him. Along the way I’ve learned some interesting facts about Islam as well. We’ve become good friends.
Training Friends and Family
The primary reason for having a trach is the ability to suction out congestion that I cannot cough up with my weak lungs. Sometimes I go for three or four days without needing any suctioning. Most days I need to be suctioned one or two times. It is most likely that I need one either early in the morning or later in the day. There is a kind of sweet spot during the afternoon that I am much less likely to need any suctioning. On a bad day if I have a bit of a cold, I can need one every half-hour or 45 minutes for extended parts of the day.
One of the requirements before they would release me from the hospital was that 2 family members needed to be trained in how to care for me. That meant dad and Carol. As a consequence when we could not get nursing help, Carol missed several days of work staying with me while dad had doctor’s appointments. It’s not just the issue of friends staying with me. I also count on friends like Rich and Kathy Logan and Judy and Anne Chapman to take me to movies, concerts, sports events etc.
I go to movies with dad and Carol sometimes but most times I go to movies with the Logans. Carol takes me to hockey games on occasion. As I mentioned earlier, I’m more likely to have suctioning needs in the evening than the afternoon so Carol and I have chosen to go to afternoon hockey games rather than evening games. Most movies are in the afternoon however some of them are around 4 PM lasting until 6 PM or later and there you are getting into the time where I’m more likely to have problems.
In addition to suctioning problems, I’m having more and more problem sitting comfortably in my back brace. By the end of the day the brace rides up under my arms and becomes more and more uncomfortable. Also I seem to have further reduced stamina so my typical day is that I do an evening G-tube feeding at about 8:30 PM and then go to bed right after that. I watch TV or work on the laptop until about 11 PM when dad comes in and puts me on the vent. I generally fall asleep about midnight or 12:30. Because of this reduced stamina and unreliability of my health during the evening, I’ve severely limited my evening activities.
We were reluctant to burden friends with the task of being an amateur EMT. However when I expressed this concern during an email exchange with Barbara Brake, she said “I would think the more EMT trained friends that you had, the better off you’d be”.
As we begin to realize that the nursing help was not coming anytime soon, we finally decided to set aside our concerns and we went ahead and trained various friends how to take care of my new needs. Psychologically this was a huge step for dad and me. Barbara Brake as well as Stu and Pat Byram now know how to do my suctioning as well as do G-tube feedings if necessary.
We also trained Rich and Kathy how to do my suctioning so that we can go to movies together. Initially the first movie we saw after getting out of the hospital was the new X-Men movie “Logan”. When you got friends named Logan and there’s a movie named Logan you just have to go. I think the first movie the three of us went to (along with some other friends from IUPUI) was “Logan’s Run”. Anyway, dad went with us in case I needed suctioning but he really didn’t like the movie. The next movie on our agenda was “Guardians of the Galaxy 2” and I knew that if he didn’t like Logan there was no way he would enjoy sitting through something as goofy and over-the-top as Guardians. So that was the final push for me to suggest to the Logans that perhaps we could train them and do it on our own. They had been waiting for me to reach that conclusion on my own.
Over this year I have missed short portions of couple of movies. Dad and I went to see “Wonder Woman” but I needed a suctioning near the end and we missed the last 15 minutes of the movie because I had to leave early and go get suctioned in the parking lot. After that, we concluded we would carry the portable suction machine into movies and other events with us. At the Traders Point Cinema there is a small, one stall, family restroom that you can go into and it’s a nice place to privately do a suctioning. Carol and I also discovered a family restroom at the Fairgrounds Coliseum where we go to hockey games. At the IMAX downtown we have just found a private corner of the lobby where we could do a quick suction. I also missed a couple of minutes of Blade Runner 2049 while Rich and I had to duck out for a quick suction. I did make it all the way through Dunkirk, Valerian and the City of a Thousand Planets, Guardians 2, Spider-Man Homecoming, Justice League, and most importantly Star Wars: The Last Jedi without interruption.
Missed Events
Although I have gotten out to some events, I’m extremely unreliable. One day dad and I were ready to go out the door to a movie and I started getting congested. We decided at the very last to simply cancel. Of course unless you buy your movie tickets in advance there is no problem with a last-minute cancellation. But for more significant events it’s been very frustrating not knowing if I’m going to have a good day or bad day. On a bad day, I need suction repeatedly and my brace bothers me to the point where I go to bed early. It’s very difficult to plan to spend $100 on concert tickets knowing that at the last minute I just wouldn’t be able to go. It seems like the fates are against me because many years there have been no concerts that I would have been interested in seeing. This year we had Billy Joel, Lady Gaga, The Eagles, the ECHL hockey All-Star game and other lesser events that in a normal year I would’ve been anxious to go to. But I passed on all of them.
Even getting to church has been quite a challenge. I’ve often described myself as a “fair weather Catholic” who only goes to church when the weather is just right. But it seems that has been even more so this year. Not only have I avoided church when it was too hot or too cold or too rainy. Anytime I’m having a bad brace day or a bad lung day I’ve chosen not to venture out to church. To get everything to line up perfectly I’ve only been able to attend mass one time this entire past year. That was just a few weeks ago on the first Sunday of Advent.
I have been blessed by a couple of visits from Father Mike occasionally accompanied by pastoral associate Claire Bain. That has helped me maintain some connection to the church in my absence. Obviously if I wasn’t making it to mass, I could not commit to teaching RCIA this year even though they did offer me the opportunity.
Assistive Technology Work
While in the hospital last December facing all of the difficulties I had with communicating, one of the main consequences of that experience was to rededicate myself to working on assistive technology. I had been promising the folks at Adafruit that I would write a tutorial on how to do Bluetooth switch control for iOS devices. Once I was back home and things were marginally back to normal I begin working on that immediately. Here is the link to that article. https://learn.adafruit.com/ios-switch-control-using-ble
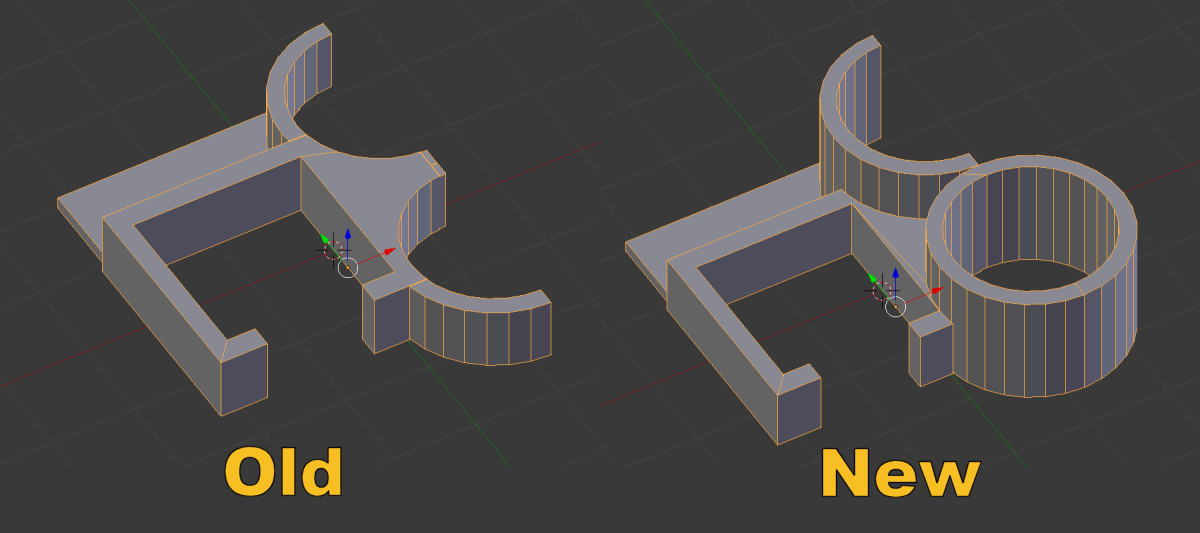
Additionally my main piece of assistive technology I use myself failed. My so-called “Ultimate Remote” had a problem and I ended up pretty much rebuilding it from scratch in March.
The Ultimate Remote is Dead. Long Live the Ultimate Remote 2.0
I also managed to meet up with an organization called ATmakers.org. This amazing organization founded and run by Bill Binko tries to match up makers, high school STEM and robotics groups with disabled people who need assistive technology solutions. Bill and I have become good friends and I’ve done a lot of work with his organization on Facebook to help answer peoples AT questions. We have some long-range plans to design an AT platform which we are going to tentatively call APHID (Adaptive Programmable Human Interface Device).
I’ve managed to get Bill and his group connected with the folks at Adafruit and collaboration has been a phenomenal experience for everyone. Adafruit has really taken up the cause of assistive technology as one of their pet projects. Bill and I have appeared on their weekly show and tell program on several occasions. Bill even was a featured guest on their Ask an Engineer program. Bill lives in Florida but recently on his way to visit a client in northern Indiana he came through Indianapolis and visited with me for an afternoon and evening. We had a great time together.
My relationship with that group is also led me to participate in various Facebook groups related to SMA (Spinal Muscular Atrophy) which is the cause of my disability. There’s a lot of activity in the field because right before the first of the year the FDA approved a new treatment for SMA that is showing great promise for infants who have SMA Type 1. The drug was also approved for older Type 2 patients like myself and Type 3 who have later onset symptoms even though there is not yet any data to support its benefits for these other types of patients. The drug is extremely expensive and administered through spinal injections. Given that it’s likely of having any positive effect on me, I’ve not pursued obtaining the treatments. I have made some good friends in the SMA community. It’s interesting that these very young children ages 1-5 who have Type 1 are approximately the same physical ability as I have as a 62-year-old Type 2 patient. They have trachs, ventilators, G-tubes etc. just like me.
I also participated in a research project by a woman from Stanford University who is studying how the use of social media is helping patients and families with SMA. It’s really amazing that we have these groups because when I was young we didn’t have these kinds of networks or support systems. We were involved in the Muscular Dystrophy Foundation when I was young (different from the Jerry Lewis MDA organization). But most of those patients and families had Duchenne’s Muscular Dystrophy which is a very different disease from what I have. So I didn’t have any information about my own disease and did not know anyone who had the same condition. It’s been really amazing and heartwarming to me to see the kind of interaction that these people are able to have that was unavailable to me when I was young.
3D Printing Activities
I’m continuing to enjoy using my 3D printer. I’ve had to repair and replace various pieces of my joystick mount for my wheelchair. I’ve created other gadgets that help mount my iPhone in such a way that I can take photos and videos with it. Mostly I’ve taken video at hockey games and some this Christmas.
I’ve also enjoyed creating just for fun objects such as puzzles, Easter eggs and Christmas ornaments. This year’s Christmas card had 3D printing as a theme. I also included a tiny 3D printed Christmas ornament in most of the Christmas cards that I sent. In some ways the ornaments overshadowed the card itself. It was one of the first completely original Christmas cards I’ve done in several years. In recent years having run out of ideas I’ve been recycling and updating older cards. My Easter eggs and Christmas ornaments have all been uploaded to thingiverse.com and have been “liked” and downloaded dozens of times.
3D Printed Christmas Tree Illuminated by Circuit Playground Express
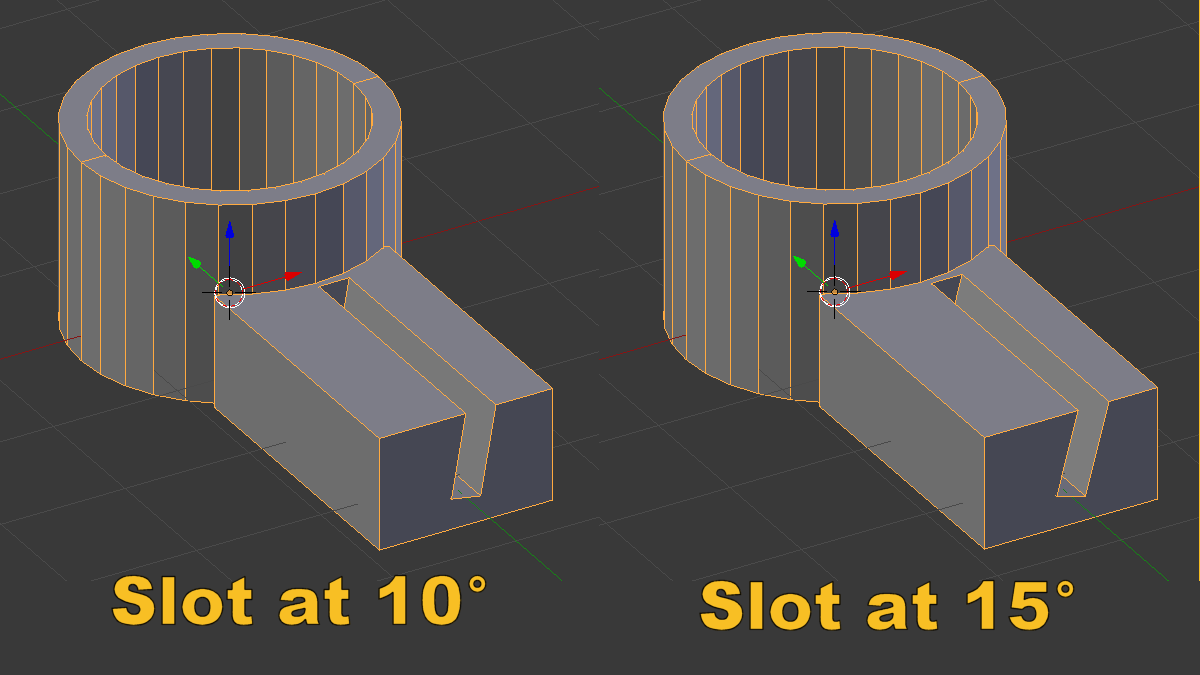
After having used Blender 3D as my CAD program of choice since I first got the 3D printer in July 2015, I finally decided to start learning Fusion 360. Blender isn’t really designed for 3D printing. It’s more for graphic rendering and animation but I chose it initially because it was open source, free, and I didn’t want to learn 2 different programs: one for rendering and one for 3D printing. But it turns out that although Fusion 360 is an expensive commercial program, it is free to use for noncommercial purposes or companies earning less than $100,000 per year. It turns out that Fusion 360 is not as accessibility friendly as is Blender. It lacks many keyboard shortcuts that I had come to depend upon. But overall because it is designed for applications such as 3D printing and because it allows you to maintain the history of creation of your designs and to make parametric designs, it is turning out to be a much better solution. The learning curve and paradigm shift have been a real challenge.
Unfortunately my 3D printing activities are going to take a brief pause because my heated nozzle quit working yesterday. A replacement part is on order. My printer is over two and half years old and will have to be completely replaced eventually. I already have my eyes on new models but I don’t really plan to buy anything new in the foreseeable future.
Programming Projects
My primary efforts in programming have been to continue the development of IRLib2 which is my library of code that allows receiving, decoding, and transmission of infrared signals using Arduino compatible hardware. It’s the basis of all of my custom TV remotes. The library has become quite popular in the maker community.
The program was originally written only for 8-bit Arduino compatible processors and I have resisted porting it to 32 bit platforms but the increasing popularity of the SAMD21 processor used in so-called “m0” platforms led me to eventually begin supporting that processor. It is used in the Arduino Zero, Adafruit Feather M0, and Adafruit Circuit Playground Express boards. I was even able to work with the people at Adafruit to get them to incorporate IRLib2 into their library of code for the Circuit Playground Express (or as I call it the CPE).
The CPE is an amazing educational platform that includes 10 Neo-pixel color LEDs, a speaker, microphone, accelerometer, photosensor, IR transmit and receive, and I forget what other features. It has also been designed to be used not only with Arduino C++ code, Adafruit is making a big push towards a language called Circuit Python. The Python programming language is used extensively to teach kids programming. The ability to run a specialized version of it on a platform like the CPE makes it an outstanding educational tool.
So once I had converted IRLib2 to run under the SAMD21 processor I decided I should take the next step and translate the entire library into Circuit Python. This was another huge learning curve and paradigm shift for me. I felt like such a noob trying to program in a strange language. In the beginning it seems like every single line of code that you write requires 20 minutes of Google searches and reading of tutorials just to write one line. Eventually you cross a threshold where you sort of “get it” and from there it’s just the mechanics of translating the code from one language to another.
Announcing IRLibCP — a Circuit Python Module for Infrared Transmitting and Receiving
There is much more programming work ahead of me. Once I got the program running on the SAMD21 platform it made sense to consider the ESP 8266 and other Internet of things type platforms. Also Adafruit is developing new boards using even more advanced m4 processors over the current m0 platforms. I will undoubtedly be spending much of 2018 working on those ports.
Blogging Activities
One of my major goals after my release from the hospital last December was to chronicle the events. I had already started writing about my experiences while still in Seton Specialty Hospital. I finally completed the story of the first days I spent in the St. Vincent ICU. The overall title of that series was “Pray That They Listen to the Man with No Voice”. While I had considered trying to get the story published somewhere other than online, I’ve not pursued that possibility. It still remains an option.
I did begin the telling the second half of the story after I was out of ICU and waiting on my ventilator approvals in the Seton Specialty Hospital. However it’s now been more than a year since those events and the remainder of that blog is incomplete. I will finish it eventually. Although not as dramatic or significant as the first part of the story, I do want to complete that task eventually.
http://mylife.cyborg5.com/long-winded-arent-i/holiday-hospital/click
I continue to do entertainment blogging writing reviews of many of the new TV shows for the fall 2017 season. I’ve not done my periodic entertainment updates as often as I would have liked.
In addition to my personal blogging, I’ve also been authorized to write for the Adafruit blog. Mostly it has been to highlight stories about assistive technology but when I come across any topic that I think would be of interest to the Adafruit maker community, I have gone ahead and posted those articles as well.
Gaming Activities
Although I have played a little online poker this past year, most of my wagering has been picking NFL games. When I landed in the hospital last December I was not able to continue to bet on NFL the latter part of the season. But so far this year I’ve been able to put five dollars on every NFL game this season. I’ve also picked three or four Notre Dame games but mostly NFL. Through week 16 of the regular-season I am up $98.71 for the year.
My biggest wins however were on an unintentional gamble. To transfer money into poker and sports gambling websites the easiest way to do so is through the purchase of bitcoin. Typically I would buy $100 worth of bitcoin and transfer perhaps $95 to the websites and they would charge me a dollar or two in transaction fees. The end result was that over the past couple of years there was about eight dollars worth of change had accumulated in my bitcoin account just from not transferring the full amount. After hearing about the huge surge in bitcoin value I decided to go back and see what that little bit of chump change was worth. Much to my surprise $8.12 had grown in value to over $142. That is significantly more profit then all of my poker and football combined. Just for fun I purchased another $50 worth of bitcoin. That should’ve brought my total to $192. At one point that value increased to nearly $230. As of this writing it’s down to $173. Of course as long as it never goes below $58 I’m still in the black. It’s kind of fun to watch it go up and down each day. I don’t plan on making it any kind of regular investment or gambling platform. I prefer to gamble on things where at least I make some of the decisions myself.
Addition to gambling, I’m also enjoying playing online browser game Travian Kingdoms. I’ve been playing various forms of Travian off and on for over 10 years. But for much of the year I’ve been seriously playing lots of Travian kingdoms. I’ve been partnered up with a great group of people from all over the world including a guy named Max from Italy and his girlfriend Kit who are great people. And my number one partner over the past couple of rounds of the game has been a college student from Poland named Patryk. Although you can play the game for free, you can get advantages in the game by purchasing something called Travian gold. I’ve spent an embarrassing amount of money on the game but I really enjoy it and I’ve made some good friends. I continued to stay in touch with Travian friends I met 10 years ago online.
Dad’s Health
Some years ago dad had a couple of spots of bladder cancer. He continues to have that checked every 6-12 months. It has not recurred recently.
Dad also has a long history of gallbladder problems. He decided it was finally time to do something about it. Gallbladder surgery was scheduled and was successful but in the process they also suggested colonoscopy which revealed some questionable polyps. That led to the scheduling of the bowel resection surgery which did discover some cancer. A follow-up with an oncologist led to a CAT scan that showed no additional cancer. The oncologist recommended not doing a more extensive PET scan. At dad’s age any chemotherapy or radiation might be more harmful than useful. So as long as the CAT scan showed nothing significant going on, they chose not to search for trouble.
Dad continues to see cardiologists on a regular basis and they discovered his heart is in an altered rhythm known as a-fib. It’s not particularly dangerous but it does put you at higher risk for blood clots leading to stroke. He went in for an outpatient procedure where they shock you back into a normal rhythm. However shortly afterwards, the monitoring of his pacemaker showed he was back in a-fib again. His chosen not to pursue any further treatment in that area.
My Additional Health Issues
As mentioned previously, the entire point of having a trach was to allow me to clear out any congestion or secretions that I could not cough up. I’m confident that had I not had the trach I would’ve been hospitalized several more times this year and possibly ended up with serious and/or fatal pneumonia. Ironically in December just about one year from my previous difficulties I did end up with a cold but because I could keep my lungs clear, it never got serious.
A few months ago I had some strange back problems. I’ve had these kinds of issues before but generally some tramadol pain pills were enough to take care of it and it would only last a day or two. This time it persisted. The tramadol and/or Tylenol had minimal effect. I was worried that even though my lungs seemed clear perhaps I had some sort of infection or pleurisy. I spent a day in the ER and they also suggested it could have been pulmonary blood clots. After a series of tests and a CAT scan they found no problems and sent me home. It was still another couple of weeks till the recurring back pain dissipated and I’m pretty much back to normal.
I still have lots of comfort issues with my back brace but I’m managing them as best I can.
Final Thoughts
As you can see, the events of 2017 don’t easily categorize into distinct issues like my usual top 10 list. Everything from my entertainment activities such as sports and movies through my maker activities in assistive technology all somehow relate to the broader issue of my trach and my health issues. So for the most part dealing with the trach and all of the consequences related to that are the one major story and just about everything else somehow is connected to or influenced by that issue.
Overall I would say it’s been a productive year where I’ve done some significant work as a maker and blogger and I’m looking forward to continuing that work in 2018.
May you have a safe and blessed new year.