Fourteenth and the last in a series. Click here for an index of all of the articles in this series.
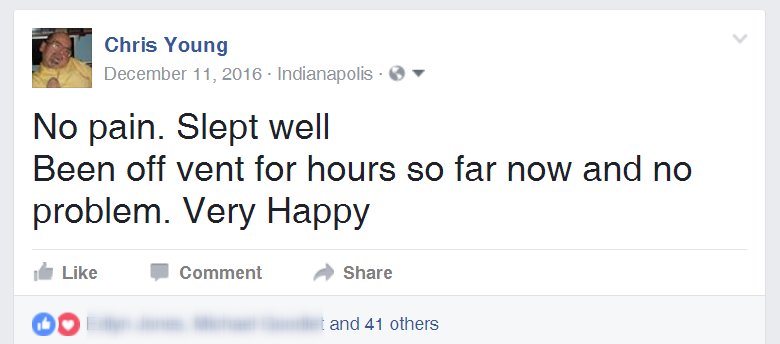
No More Cloud
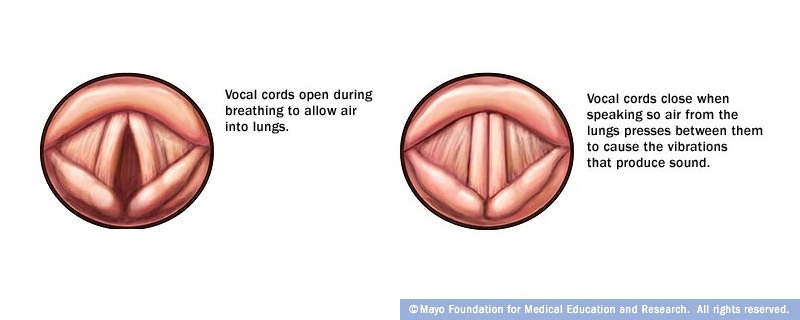
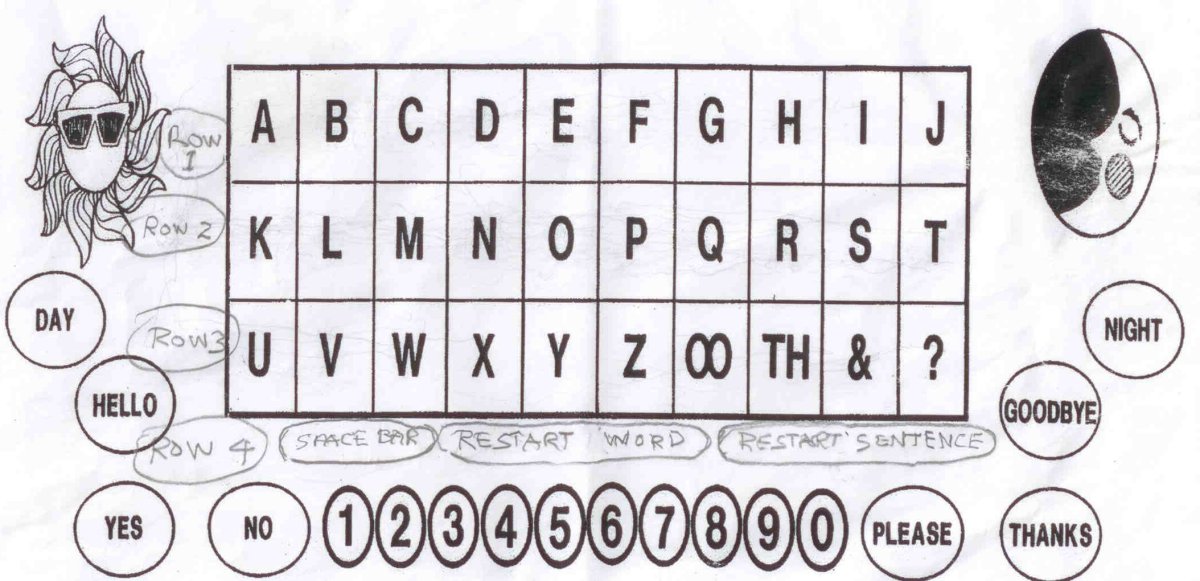
In our previous installment I had an emotional meltdown over by inability to talk with the trach. I was facing a wide variety of issues that need to be resolved. Not being able to talk and to participate in the decisions was a real mess for me. When I finally got the talking valve late in the afternoon of December 12, I still had lots of issues to deal with but at least I could now actively participate in those decisions. It’s hard to say that there was any advantage to not being able to talk but the fact that we had to type everything on my iPhone into the Notes app did give me an archived record of everything that I had typed. All of the messages were saved in my iCloud account. Even though I deleted them, they remained in the “recently deleted” folder for 30 days. When I had realized what a resource those messages were for piecing together this blog, I restored all those recently deleted items into a folder called “formerly deleted” and I’ve used those messages to help piece together the story. Put that together with my Facebook posts and I had a pretty accurate blow-by-blow picture of what I had been through. Now that I was talking, there was no more permanent record in the cloud. It’s taken me so long to get to this point of writing the blog that it’s more than three months later so my memory is a little bit fuzzy on details.
Outstanding Issues
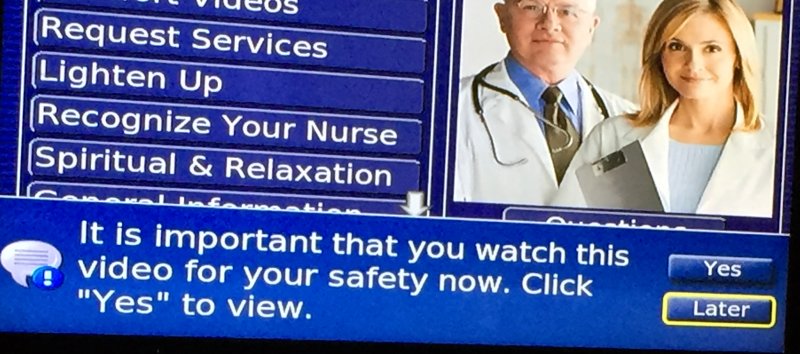
Even though I didn’t have the benefit of an iCloud archive, I did seem to have a lot of clouds hanging over me with all the issues that needed to be resolved. Once the valve was in and I could speak I could begin dealing with issues one by one. I suppose the biggest issue was if I was going to need a ventilator to replace my CPAP so that I could sleep. I had proven many times in recent years that I simply could not sleep without a CPAP. For example if there was a thunderstorm and our power was out overnight, I had a backup oxygen tank to replace my oxygen concentrator but I had no way to operate the CPAP without power. Despite my best efforts to sleep under those circumstances I could not do it at all.
On the morning of the 13th I got off of the ventilator and put in the talking valve. Sometime during that day I tried to take a nap without any mechanical assistance. Much to my surprise I was able to doze off for about a half-hour or 45 minutes without the ventilator or a CPAP. That was very surprising. However the experience did tell me that I wasn’t sleeping well enough to really sleep through the night. I explained that to the doctors and they all agreed that yes I did need a ventilator at night to replace the CPAP. They begin to understand that I have been using the CPAP not only to open my upper airway but to assist with keeping my lungs inflated. So then we had to go about the process of getting the ventilator for my home.
There was a woman who was my case manager. It was her job to get whatever I needed to get me home. As I mentioned previously however, the process of getting an in-home ventilator was theoretically going to take a full two weeks. At first I thought the delay was because it took that long to get some sort of Medicare or Medicaid approval. Actually that part was relatively easy. It was just logistics of finding the right durable medical equipment provider and jumping through a bunch of hoops necessary to get the equipment. Among the things they wanted to do was to inspect my house electrical system to see if it was sufficient to handle the equipment. It turns out this was a totally ridiculous requirement. The ventilator doesn’t require any special electrical capability. It probably uses no more current than an ordinary CPAP machine. The problem is that once you say the word “ventilator” it raises the image of someone who is dependent on the thing to stay alive. The image is of a person who will die within minutes if the ventilator fails. It turns out that this ventilator has a battery backup that is good for several hours so even if I was in a life critical situation, electrical failure wouldn’t be fatal. In my case I’m NOT in a life critical situation. In fact I’m less dependent upon the ventilator than I was on the CPAP. However none of that mattered. We still had to jump through all the hoops.
The case manager was initially talking about using a company called Apria Homecare which is one of the biggest equipment providers in the area. Years ago I had got my oxygen equipment from them but they were a little bit difficult to deal with and we ended up changing to a different company. I was willing to go with them despite my previous bad experience so I didn’t say anything against them. Then the case manager came back and said she was going to try a different company that was an independent small company run by a respiratory therapist. I forget the name of the company. I like that idea because I had recently changed to a different home health aide agency that was a relatively small organization. I had felt like I was getting more hands-on attention from a small group that I had with the larger company in the past. So the idea of a small operation for the ventilator provider was attractive to me. Unfortunately somewhere along the way she came back to tell me that we cannot use either of them because different durable medical equipment companies have contracts with Medicaid to cover certain geographic areas. It turns out that I had to use Home Health Depot because they had the Medicaid contract. But we didn’t find that out for a couple of days. That delayed the entire process even further.
The next issue to deal with was that I wasn’t sick enough to be in the ICU and I could not be transferred to a regular room because they don’t allow ventilators on regular medical floors of the hospital. So the alternative was to transfer me to a long-term critical care hospital also known as St. Vincent Seton Specialty Hospital named after St. Elizabeth Ann Seton. She was the founder of the Daughters of Charity of St. Vincent de Paul. They have founded a number of institutions including the St. Vincent Healthcare System. Seton Specialty Hospital was just a couple blocks away on Township Line Road. So we began making arrangements to have been transferred there. It would probably happen on Wednesday the 14th. I asked the doctors directly “If I had all the medical equipment that I needed at home, when do you think I would be medically ready to go home?” The doctor said perhaps two or three days. So that meant I was going to spend 9 or 10 days in this other hospital unnecessarily just because we could not get the logistics of getting me a ventilator at home.
And people wonder why healthcare is so expensive.
The final issue I needed to wrestle with was that I now had a urinary Foley catheter stuck in my stomach instead of a proper G-tube. I made it clear to anyone who would listen that I wanted this issue resolved. I came into the hospital with a proper G-tube that had the proper kind of valve on the end of it. I intended to leave there with the same kind of G-tube. I wanted someone experienced in replacing the tubes. If we had to go down to the radiology department to use x-ray assistance then that was okay with me. In fact I would prefer it. That’s how they’d put the tube in to begin with. We had tried 2 different sets of incompetent surgical residents who couldn’t seem to get a tube in properly. They finally agreed that on the morning of Wednesday the 14th they would take me to the radiology department and replace the Foley with a real G-tube.
Other Loose Ends
In addition to dealing with the case manager, I spent a fair amount of time with the young resident Dr. Heaven. She had really appreciated my emotional state when I was demanding the valve and was instrumental in getting everybody to agree to it. One of the questions I had for her was where was the medical student Brady who had sort of been my other go to guy when trying to resolve problems. She explained that he had taken a few days off to study for his residency exams and then would be taking exams. I was disappointed that I wasn’t going to get to see him again before I left for the other hospital. Fortunately I did reconnect with him later. After I got home, I got an email from him saying that he had found my blog. We swapped a couple of emails and became Facebook friends. He has been following this blog with great interest. By the way he passed his residency exams and was accepted into a residency program in a military hospital in California. He was really looking forward to it. He had been in the military previously.
Sometime on the 13th or the 14th before I left St. Vincent, I had my second conversation with the nursing supervisor about the way I had been treated and my wishes being disrespected while I was unable to speak. I had already recounted that story in previous installments but this is when that second conversation actually occurred.
The Most Interesting Doctor in the World
On the morning of the 14th they took me down to the radiology department to finally replace the Foley with a proper G-tube. They rolled me down to a waiting area that I was familiar with. This was my third trip to that particular department. The first was one time in 2006 when I was in for my intestinal problems. They had inserted a central line in my carotid artery. The other time was last May when I had the G-tube the first time. After a brief wait the doctor arrived. The instant I saw him I thought to myself “I bet the ladies around here are going absolutely nuts over this guy.” He looks like the kind of doctor that you would see on a medical TV show and could’ve easily replaced Patrick Dempsey on Grey’s Anatomy and be given the title “Dr. McDreamy”. He was Hispanic at about 5’10”. He had black hair and a short neatly trimmed black beard and mustache. It was so precisely shaped it almost looked like it had been cut out of black felt or velvet and been glued onto his face. He had on scrubs for pants but he was wearing a tight fitting “UA” brand athletic shirt made of some slick material with lots of tiny holes poked in it. His upper arms were massive it looked like he worked out in the gym eight hours a day or something. In some ways I thought of him like a 35-year-old version of the Dos Equis “World’s Most Interesting Man”.
I will fast-forward till after the procedure when I asked a couple of the nurses if he was really popular and if the nurses had a crush on him. They told me that they probably would have except that he already had a very hot looking wife and a couple of gorgeous young children. That didn’t surprise me at all. I jokingly described him to one of the nurses as “He’s hot enough to turn a straight man gay”. One of the nurses came back with “Or to turn a lesbian woman straight.” We all got a big laugh out of all that. Disclaimer: I don’t really think you can turn someone gay or straight. It’s not a choice. People are wired gay or straight. We were just making a joke about what a hunk this guy was.
Anyway he questioned me why I wanted the tube changed. I explained “Look there are two different kinds of tubes. There are Foley catheters for your bladder and there are G-tubes for your abdomen. They wouldn’t have invented two different kinds of tubes if they didn’t really have a difference to them. I’ve been using a G-tube with a valve on the end of it ever since May and it works out really well for me. The Foley just has a cap with no valve. The stupid surgical residents couldn’t get a regular G-tube put back in. I don’t know what they were doing wrong but it hurt like hell. You need to numb me up so it doesn’t hurt, use the x-ray as a guide, and put in the right kind of tube.” He said okay as if he appreciated the guy who knew what he wanted and wasn’t going to take no for an answer. They wheeled me into the procedure room which was also a very familiar place from my two previous experiences. A couple of shots of lidocaine took care of any pain and the tube was replaced in no time.
I thought that that was the end of it until someone got to looking at the tube and there was speculation that they had put the wrong kind in. A traditional G-tube goes a short distance into your stomach and is used for people like me who have swallowing difficulties. However if part of your problem is digestive, there is a different kind of tube called a J-tube that extends down into your intestine. There is also a combination G-tube and J-tube that is a two-in-one device. Because the valve on the end of this new tube had 2 ports on it, some of the people who looked at it thought that it was perhaps one of these combo tubes. We didn’t do anything about it at St. Vincent but the issue got raised later in the day when I was transferred to Seton. They thought perhaps the people at Seton were going to have to replace it again. As it turned out it was not a combo tube. It was just a regular G-tube with 2 ports. It did not need replacing again and the tube has worked flawlessly ever since then.
The rest of the afternoon was sort of a “hurry up and wait” situation. I was going to travel by ambulance from St. Vincent ICU to St. Vincent Seton Specially Hospital but we didn’t know exactly what time it would be. I was one of 2 patients who were going to make the same trip. Of course it always takes a lot of paperwork to discharge someone. Transferring them to a different hospital is no exception. And to have 2 patients from the same department making the same trip also kept the nurses very busy. Eventually it was my turn. They loaded me onto a gurney and wrapped me up in a bunch of blankets. The ambulance trip took only five minutes or so. Getting in and out took longer than that. My notes tell me that I posted on Facebook at 5:19 PM that I was settled in to room 207 of St. Vincent Seton Specially Hospital.
Final Thoughts
That essentially wraps up the story of “The Man with No Voice”. It was most definitely the most emotional and stressful hospital experience I’ve ever had. The repercussions of it will carry well into the rest of my life. However I think the story of my adventure at Seton is sufficiently different that it is a story unto itself. It’s not nearly as dramatic and there will not be as much detail to talk about. I will get to work on writing it very soon. The brief story is that I spent from the afternoon of December 14th until December 28 at Seton. It did take exactly 2 weeks to get the ventilator ready for me to go home. If not for the logistical nightmare, I could have been back home within a few days.
I still am amazed at how differently I was treated when I couldn’t talk. I’m still a bit haunted by the fact that there are many, many people who face these challenges every single day of their life. I struggled with it for a little more than a week and it nearly drove me nuts. I spoke of the surprising level of commitment and support from my friends in the maker community especially those at Adafruit Industries. One of the consequences of this experience was that I was recommitting myself to developing assistive technology not just for myself but for other people. For example for months I had promised to write a tutorial about how to do switch control using an Adafruit Bluetooth device and an iOS device such as iPhone or iPad. One of the very first things I did once I had settled back in at home was to finish that tutorial. I’ve also connected with another group called ATmakers.org which is run by a man named Bill Binko. His organization is working with high school STEM programs to encourage kids to use their science, technology, engineering, and math skills to assist disabled people with their assistive technology needs. I now have a very deep commitment to make sure that everything I know about assistive technology gets passed on to other people who can make use of it. The folks at Adafruit have also taken up assistive technology as one of their pet projects. They are working with me and Bill to develop new devices that will be of use to the AT community. Now that I have my voice back, I’m using as much of it as I can to give voices to others who have no voice.
You can click here to read my other series titled “Holiday Hospital” about my experiences recovering over Christmas at the other hospital.