This is the fifth in a continuing series of posts about my experience (limited as it is) as an author. Click here for a complete index of all the stories in this series.
I’m celebrating today. I got my first rejection letter!
I’ve not had a lot of things published but I have published a few. I’ve been talking about them in this series of blog posts that I’m calling “Author’s Journal”. I’ve got more articles to write in this series about things that have gotten published. And then something happened today and I simply realized it had NEVER happened before.
I got a rejection letter. (Actually it was an email.)
Anyone who has ever tried to sell their written works probably has enough of these to wallpaper their entire house and then some. Every bit of advice I’ve ever heard about writing is that getting rejected is something that’s going to happen a lot. I ran into a guy on Facebook who had written some sci-fi stories and he got 50 rejections before he had his first sale. But for some bizarre reason (and certainly not because I’m such a brilliant writer) until today I’ve never been rejected. I never thought about the fact before. I never realized how extraordinary it was.
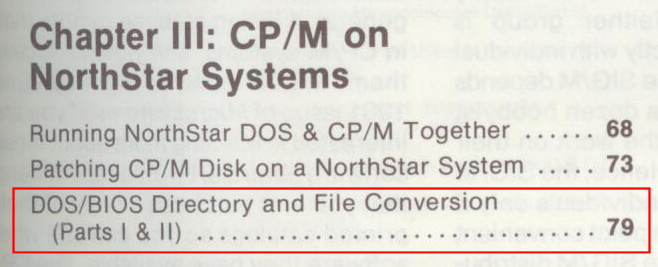
Let’s take a quick review of the things I’ve published. In a previous blog post I talked about 2 technical articles I wrote for an obscure computer magazine called “Microsystems”. They were a couple of little file conversion utilities that I had written for computer disk systems that no longer exists. If there had been the Internet back in those days it would’ve been a couple of simple blog posts and maybe a dozen people might have stumbled onto it if they had done the right Google search. But because these niche magazines in the early days of personal computing were so anxious for content, they agreed to publish my first article and a few weeks later I submitted part two and they brought it as well. They even republished the magazine articles into a book that was sort of a “best of” collection even though the title didn’t say that. Read my blog below about how inappropriate it was for my articles to be in that compilation and the story behind the story.
The second thing I had published was my autobiographical article “The Reunion” which was published in the September 1987 issue of Indianapolis Monthly Magazine. It was a memoir of me growing up attending a special education school called James E. Roberts IPS School #97. They had a reunion at the school that I attended to celebrate that it was closing and all the special ed kids were being mainstreamed into regular education. The visit to the old school brought back lots of memories and I chronicled them in that article. While “Microsystems” was anxious to publish my technical article, Indianapolis Monthly very nearly rejected my story. You can read the story behind the story of “The Reunion” in this post from Author’s Journal which also includes links to an online version of the original magazine article.
My next published work was a book that I contributed to called “Ray Tracing Creations” about ray trace computer graphic rendering. I was part of a team of volunteer programmers who built an open source rendering engine called POV-Ray. The team leader, a guy named Drew Wells, got the contract to write a book about our program. He got tied up in his personal life and only wrote about five chapters and couldn’t finish it. Because I was the next most experienced and knowledgeable person on the team, they reached out to me and I wrote the rest of the book. A short time later we did a second edition rewrite and I got top billing over Drew. It’s not like I wrote something on my own on spec, submitted to a publisher, and waited for a reply. So in this case there really wasn’t a chance of a rejection letter unless what I wrote was just so awful that they decided to scrap the entire existing project. I’ve not yet chronicled the story behind that story. Look for it in upcoming blog posts.
I also had a second magazine article published in Indianapolis Monthly about my first time attending the Indy 500. Although I had been a lifelong race fan and been to practice and qualifying countless times my entire life, I had not yet attended the race itself because prior to that there wasn’t a good place to sit in a wheelchair. The story behind that story will be featured in a future Author’s Journal. While this story could have been rejected, they already knew me and liked my work. This story about my first 500 wasn’t as emotional or moving as “The Reunion” but it was good enough.
Since then I’ve been doing technical writing for the Adafruit Learning System in which I talked about various maker projects I have created most of them involving assistive technology for the disabled. The folks at Adafruit were familiar with my projects because I would show them off on their weekly video show and tell chat room. They had also seen some of my technical blogs and they were happy to publish my articles. Initially I was paid in free merchandise but more recently have been paid monetarily. Again this was a situation where they knew my work, they were anxious to have it, and the chance of getting completely rejected was relatively small. Click here for a list of my technical articles on the Adafruit Learning System.
Some of my best writing has been in my personal blogs but of course I’m the publisher. I’m not going to reject my own work 🙂
This entire Author’s Journal is being written because last summer I decided to try my hand at writing fiction specifically science fiction. I’ve written a novella that was initially 24,500 words long. The problem is the major sci-fi magazines like their novellas in the neighborhood of 20,000-22,000 words long. I worked hard to get it down to 22,000 but that still is going to limit my market.
While I was working on that, I had a dream and when I woke up from it I had the idea for a short story. A very short story. Just 300 words. That’s too short. Some of the sci-fi magazines publish extremely short things under the category of “Poetry” and although it wasn’t necessarily written in verse and did not rhyme, it did have a sort of lyrical poetic nature to it. Maybe it was free verse. Maybe it was a very very short story. I didn’t know.
I was so excited that I had been inspired to write this clever little short piece and had not planned on writing that I did way too little research on where I should submit it.
The obvious choice was the “Magazine of Fantasy & Science Fiction“. It was a little bit surrealistic and so it was more fantasy than sci-fi. Unfortunately at the time they were in the process of changing editors and had closed the magazine to new submissions until they published their backlog of purchase stories and sets of new editorial goals under the new leadership. My favorite of the top sci-fi magazines is “Analog Science Fiction – Science Fact Magazine” but they mostly publish what we might call hard science (technology, spaceships, computers etc.) That left “Isaac Asimov’s Science Fiction Magazine” as the remaining one of what I would describe as “The Big Three”.
The story took me less than a half hour to write. I spent less than an hour deciding Asimov would be my first choice. I uploaded it with a note saying “I don’t know if this is poetry or a very short story but I thought I would submit it anyway.”
They say wait five weeks for an answer. I was also supposed to get an email acknowledging the submission which I never got. But when I would go to the submission website and type in my receipt number it said that my story had been received.
Shortly after submitting it, I discovered there was an entire category called “Flash Fiction“. It consists of extremely, extremely short stories never longer than 1500 words. Unknowingly I had written flash fiction which Asimov typically doesn’t publish. It turns out that Analog does publish flash fiction occasionally. They had one in their November/December 2020 issue. But again this wasn’t sufficiently hard science Analog-like.
I did find an online webzine that pays professional rates of about eight cents per word. It’s called “Daily Science Fiction“. They publish a new story every day that comes to you free by email or you can go to their website. Everything there is flash fiction under 1500 words and preferably under 1000 words. Perfect for what I had written. They publish all sorts of speculative fiction including sci-fi, fantasy, and another category I had never heard of cald slipstream. Apparently slipstream is sort of a bizarre otherworldly kind of writing that is not mainstream but slipstream. Maybe that’s what I wrote.
Realizing how inappropriate my choice of Asimov was, I was a bit anxious to get rejected so that I could submit it somewhere else. It is strictly forbidden to submit the same item to multiple publishers at once. If they catch you, you could easily get blacklisted. Maybe not from the whole industry but certainly ruin your chances with the publications involved.
When the five-week waiting period was up, I still had not heard back anything from Asimov’s. They said if you don’t hear anything after five weeks that you can email them so I did.
Again I explained that I didn’t know if what I had written was poetry or perhaps flash fiction… Probably the latter. But they said if you don’t hear anything in five weeks I can email you so here I am asking what’s my status. Then I added a paragraph… It said something like “By the way I’ve got this novella. Your guidelines say that you ‘Rarely publish anything over 20,000 words.’ I’m working on a novella that I’ve managed to trim down to 22,000 words. I suppose if I was an established author you might stretch your limits but has a guy like me who is unpublished got a chance with a 22,000 word story?”
I fully expected them to write back saying “The rules are the rules. Go away kid… You’re bugging me with this 22,000 word crap.” Much to my surprise I got a very nicely worded email explaining that poetry goes to a different editorial process and can take up to two months. And that my novella wasn’t extensively over the limit and they suggested I go ahead and submit it. They said if we like it and it’s too long we will help you cut it.
I had been through that before. “The Reunion” was too long and the editor there gave me another chance to trim it and then she trimmed some more and put back in some things I took out. So it was a bit of déjà vu.
I still had some final edits to do on my novella but my plan was to submit it at 22,000 words and see what happens. A friend of mine is doing some final proofreading for me and I should be ready to submit it very soon.
Meanwhile today Asimov finally rejected my flash fiction. I was so happy. Now I can send it somewhere more appropriate and have a better shot at it. I have submitted it to Daily Science Fiction. They say that they try to respond quickly but if you haven’t heard anything in four weeks you can contact them. There is a place where you can look up the status of your submission online. So now we wait and see. Maybe I will get another rejection which is okay.
Also over the weekend I finished the first draft of a sequel to my as yet un-submitted novella. This one has come in at 16,000 words so I won’t have to do any major surgery on it to get it within the standard writers guidelines.
I will keep you posted as the story develops and I will be working on more installments of Author’s Journal telling the stories behind the stories of what I have published.