Tenth in a series.Click here for an index of all of the articles in this series.
Being Human
We are now up to Friday, December 9th which turned out to be a very busy and eventful day. It’s probably going to take me two or three blog entries to cover the events. The first thing on the agenda that morning when dad arrived was that we wanted to try to shave me. Unless I’m going somewhere public, I typically only shave every two or three days just because it’s a hassle. I had been in the hospital for six days and I really don’t remember how long it had been prior to that that I shaved. So I was getting very grungy.
Because my neck is so short it’s hard to get a razor under my chin. It’s even more difficult to do so when I’m lying in bed. With the help of a nurse, dad raised me up in bed and stuffed a pillow behind my back so that we could tilt my head backwards and he could shave me. Even though they had been giving me a bed bath every day they didn’t always wash around my neck very well. So the first thing we did was have the nurse thoroughly wash my neck and get around the trach tube carefully. We laid a wash cloth over the opening to my trach while dad shaved me with my electric razor. It was a very awkward position but we managed to get me shaved. It felt good to get all of that off of my face. I almost felt like a human being again.
Unfortunately in the process I’m pretty sure we did something to kink my back. Later that night I had pretty severe back pain. When I get that pain I’ve been taking a pain pill called Tramadol but when I tried it that night it was not enough. I ended up having to take Fentanyl which is a pretty strong narcotic.
The other bit of “cleaning up” that I got that day was a visit from the hospital chaplain priest. When Fr. Paul had visited me a few days earlier I had not asked him to give me the sacrament of Anointing of the Sick because I thought I was on the mend. But when it became obvious I was going to have trach surgery and I was still a long way from full recovery I had asked the chaplain to send the priest to give me the sacrament. This isn’t necessarily because I thought I was dying. You can get the sacrament anytime you are seriously ill. I don’t recall the name of the priest who came by but he gave me the anointing. I had pre-typed a message on my iPhone that was a sentence or two of confession. He read the confession but said don’t worry about it that an anointing is just as good as confession. I had heard that before but I thought I would go ahead and mention a few things that had been on my conscience. That’s one message that I completely deleted and did not recover on my iCloud archives. Afterwards I posted a message on Facebook saying “Just got anointed by the priest, let the healing begin!”
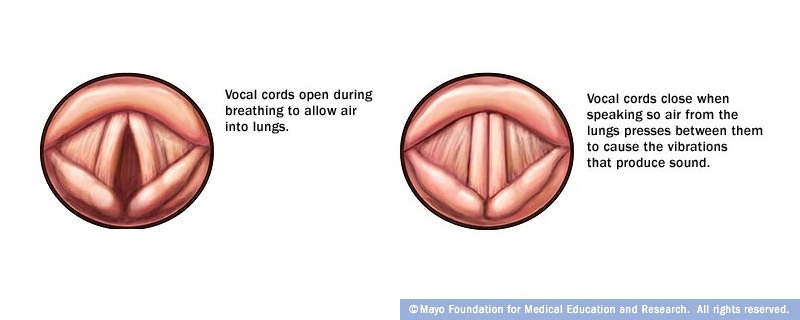
As I had done the day before, they tried taking the off of the ventilator and letting me just breathe normally through the trach. The day before I had been off for several hours and only needed to be suctioned perhaps twice. This day I was in much worse shape. After only 15 or 20 minutes off of the ventilator I needed to be suctioned with a catheter. I thought I was cleaned out but after another 15 or 20 minutes I needed it again. It was just too much of a hassle if I was going to need that much suctioning. I decided to give up and we called the respiratory therapist to put me back on the ventilator for the rest of the day. It was a very frustrating and disappointing day for trying to get clear of the vent.
Here We Go Again
Disclaimer: I’m going to be brutally honest in this next section about my thought processes. I’m likely to come across as an insensitive, misogynistic, male chauvinist pig. I don’t really think I’m any of those things. I love women. I respect women. I enjoy looking at attractive women. The hard facts are I’m a 61-year-old horny old guy. That doesn’t mean I only see women for their physical attributes. I don’t believe I objectify women. Any of my female friends who can say they’ve seen a hot looking guy walk by and they NEVER took an extra long look at him and wondered what a physical encounter with him might be like… then they might be able to sit in judgment of me. But all of you other ladies who have ever done any guy watching… don’t judge me.
I mentioned previously that when I need to suction the trach with a catheter it had to be done by an RN. One of the times that I needed to be suctioned that morning, my regular nurse who is familiar with me was not available so they rounded up someone else to do it. This nurse who I had never seen before was actually one of the hottest nurses I had seen since I’ve been there. She was very tall, athletic build, light brown hair with blonde streaks in it, probably 40 years old or so. I’m a bit embarrassed to say that if I had to describe her in one word it would be “MILF”. I know that’s a very misogynistic, chauvinistic label to apply to a woman but I mean it with a great deal of respect. I don’t think the term (at least as I apply it) objectifies women. It simply expresses that I found her to be a mature woman who was very attractive in a physical sense.
She did a competent job of suctioning my trach tube and then she looked at me and said “You are slumping down in the bed. We need to scoot you up higher.” The problem was I had just recently gotten comfortable in that position. I had already been twisted and turned in unusual ways to try to get me shaved earlier. My back was hurting unless I would sit just right. I definitely did not want to be moved.
The nurses are rightly concerned about pressure sores developing on my rear end. However in my experience some of the things they do to alleviate pressure actually cause me extra pressure. If they grab you under the arms and slide upwards to keep you from slumping, your natural tendency is to slip downwards again. But you’re butt naturally doesn’t want to slip on the sheets as your body is trying to slide down and forward. It creates a sheer force on the soft part of your buttocks and on your tailbone. That sheer force on your rear end risks more pressure sores rather than alleviating them. I do much better if I’m slumped a little bit even though I look strange in that position. Add to this the fact I have very severe scoliosis and I was in bed without my back brace. That makes me look even more slumped than I actually am.
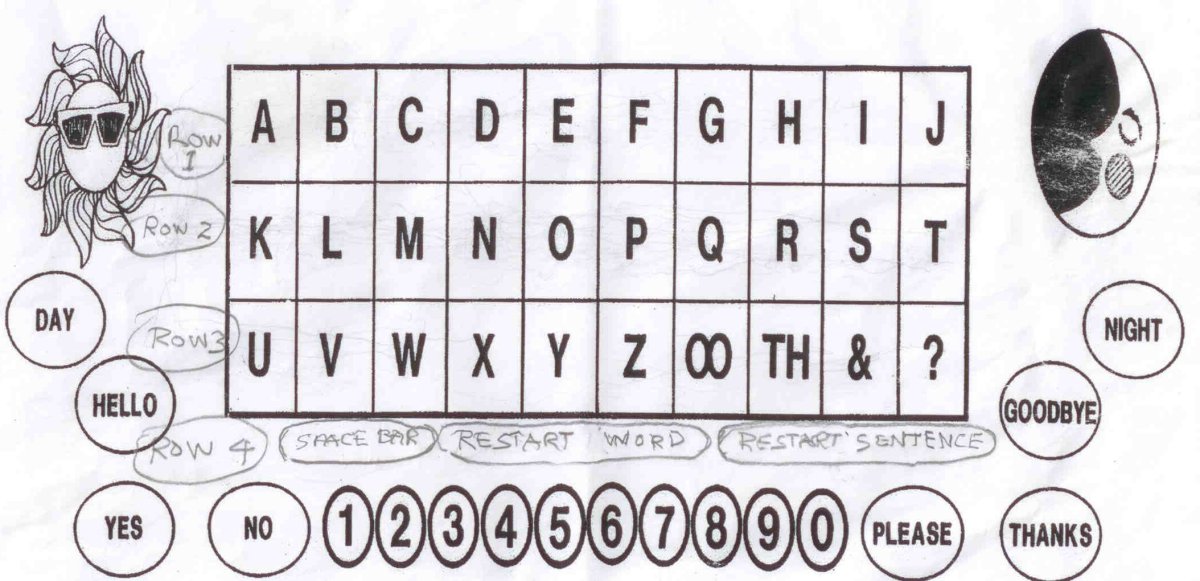
When she suggested scooting me up in the bed I began giving my “No” signal indicating that I did not want to be moved. I was certain that she understood my signal because she argued back at me insisting that I needed to be moved. At one point my dad said to her “He’s saying ‘No'”. It was to no avail. With the assistance of one of the patient care techs they grabbed me under my arms and pulled me up higher in the bed.
They didn’t hurt me. But they moved me out of a very comfortable position into an uncomfortable position for no good reason and over my explicit objections.
In what I called “The First Incident” I was absolutely furious and a little bit scared. In this second incident I just felt frustration, disappointment, and a sad feeling that it had happened again. When something happens one time you can write it off as an isolated incident. But when it happens again you begin to realize that this is just the way things are for people who cannot communicate and who are dependent upon caregivers.
I thought about getting on the iPhone and writing a really angry message and then getting someone to bring her back to read it. But I just did not bother. I guess I would just have to make another appointment with the nursing supervisor and issue yet another complaint.
I think part of it pissed me off that I had found her attractive and then she turned out to be such a bitch. What gave her the right to violate me in such a way? Just because I thought she was hot doesn’t mean I would’ve run up and grabbed her ass if I had the physical capability to do so. I’m not a misogynist, chauvinist pig. I respect women. I understand the concept “no means no”. All I could think of was God help her if she ever ran into a guy in a dark parking garage who had her same disrespect for the meaning of the word “no”.
Okay now you’re going to say how insensitive I’m being by equating sexual assault to getting my ass moved in the bed. That’s not what I’m saying. I’m saying that “no means no” in all circumstances big and small.
We will fast-forward to Tuesday or Wednesday the 13th or 14th when I was able to talk again using a special talking valve on the trach tube. I asked to speak to the nursing supervisor and complained again that one of her nurses had ignored my refusal to submit to something I thought was unnecessary and had no true medical purpose. I reiterated to her that it wasn’t like I was some sort of Alzheimer patient who didn’t really know what was going on. That I had the right to determine what did or did not happen to me as a patient. In this instance I was able to communicate that I did not want to be moved. I was not able to communicate a lengthy explanation why. But I should not have needed to. I said to the supervisor clearly “I understand the concept of ‘no means no’ and that I would think that a woman would appreciate that and treat me with the same respect that women expect from men.” I did make it clear to the nurse yet again that I had not been physically hurt nor psychologically scarred but I felt violated nevertheless. She agreed it was unfortunate situation that would be addressed again.
The Bigger Issues
There is a natural tendency to see someone with a physical disability and somehow presume some sort of diminished mental capability as well. That unfortunate presumption multiplies a hundredfold when the disabled person cannot speak. My late friend Christopher Lee whom I’ve spoken of earlier in this blog had an experience where he was sitting somewhere in a public place in his wheelchair with a lap tray on. Someone walked by and place money on his tray as if he were some sort of beggar. It was just a dollar or so. The childlike tone with which people would address him was commonplace. He said he could endure such insults because one time someone also mistakingly took him for being Stephen Hawking. So to him being mistaken for a mentally handicapped beggar got balanced out by being mistaken for being the world’s most famous genius.
A condescending tone is something I’ve experienced on a regular basis from strangers. My number one weapon against all that has been that I speak up and reveal myself to be articulate, educated, and in all other nonphysical respects a normal or above normal human being. I always understood that that defense was not available to people like my friend Christopher and was saddened by the fact that he had to endure such things. However I was getting a whole new appreciation of the kinds of things that Christopher and other non-communicative disabled people face on a daily basis.
In telling the story to friends and family and in describing the incidents to the nursing supervisor I’ve said things like “I’m college educated. My IQ came within two points of being eligible to join Mensa. I’m not an Alzheimer’s patient or a stroke victim or dementia victim who doesn’t know where they are or what they are doing, I’ve been dealing with this disability for my entire 61 years and I know my body better than anyone” etc. etc.
But somewhere along the way it occurred to me that that argument was a bit bogus. What if I wasn’t as smart or articulate or is experienced as I am? What if I was an Alzheimer’s patient who barely knew where I was or what was going on around me? At what point does having a mental deficit mean that it’s okay to deny me my rights to determine what happens to my own body? How mentally impaired does one need to be before they are no longer permitted to refuse nonessential care from an insensitive caregiver?
I began to feel a little bit guilty that I presumed that only smart, articulate people had the right to self-determination. People with dementia and other mental impairments suffer enough indignity as it is just because they are at times clueless as to their condition, surroundings, and entire state of being. Must they also suffer the indignity of not being able to direct their own physical care at least in noncritical circumstances? My experience in these two incidences lead me to conclude that they probably are treated in significantly disrespectful ways. My defense that I’m awake, alert, and ornery times three makes me guilty of looking down upon and disrespecting dementia patients as much as the people I’m railing against.
If I’m characterizing myself as “the man with no voice” to which no one is listening, how much more so are the dementia patients voiceless and unheard?
To be continued…