Before I start on this blog installment, I’m going to try something a little bit new. Every time you see this little  Facebook logo, you can click on it to see a post that I put on Facebook as these events were occurring. Now on with our regularly scheduled story…
Facebook logo, you can click on it to see a post that I put on Facebook as these events were occurring. Now on with our regularly scheduled story…
The previous blog in the series can be found here
Tough to Swallow
When I left off in a previous entry on May 2, I had told the story of my decades long problems with swallowing, I said that I was going to call the doctor for an appointment to talk about the possibility of getting a G-tube. In this lengthy blog post I will talk about what I went through to get the G-tube and the complication of having a urinary infection that sent me to the hospital in the middle of all this.
I did call on my doctor that day and made an appointment for Thursday, May 12 with my primary care physician Dr. Jeffrey Kyrouac.
G-tubes and Breathless and Lawsuits… Oh My
I mentioned that it was a very stressful time for me with my new wheelchair, new caregivers coming and going every few weeks, and the stress of not being able to eat very well. That stress all multiplied on Wednesday, May 4 when I got an email from a photographer threatening to sue me for copyright violation. I had used a photo of the Indianapolis skyline at night as the background for my 2013 computer-generated ray-traced Christmas card. The short version of the story is that both I and my lawyer tried to negotiate a settlement and it went nowhere. The guy eventually filed suit in federal court and as I write this blog post in late June we are about to file our response. My lawyer since I have a good chance of a “fair use” defense. When the complete case is over with I will blog about it extensively but for now it’s best if I don’t discuss the case. I just mentioned here to give you an idea of the added stress that I’ve been having.
Note: After several months of negotiations and extensive legal costs we reached an out-of-court settlement and I purchased a license to the image. I need to write a blog about that entire process someday but some of it is under a nondisclosure agreement.
I went to the doctor on the 12th expecting to discuss with him what my options were short of actually getting the G-tube. His attitude was that I had been using all my options for the past 20 years and now there was only one option and that was to get a G-tube. The really wasn’t any debate about it. It was a tiny bit of a wake-up call for me. His attitude was like “Hell yes you need a G-tube” and I suddenly realized “Hell yes I DO need a G-tube. What was I thinking?” So he referred me to a gastroenterologist.
The next day was Friday the 13th and in some ways it was a bad luck day. Part of my morning routine is after getting a bed bath we occasionally hook me up in the Hoyer lift and sit me on the toilet. I hang in the sling for a few minutes and when I’ve done my business I call for dad or my home health aide to get me. But for some reason on this particular day I was hanging in an awkward position and I couldn’t get enough breath to call them. Sometimes it can take as long as 10 minutes for me to finish so dad wasn’t concerned. The new caregiver had no experience to know how long I might be. Finally after about 15 minutes she came to check on me and I whispered “Get my dad”. When he got there I whispered “I can’t breathe”. He rushed me back to bed and I was okay after that. It wasn’t that I really could not breathe. I wasn’t at risk of passing out. But I could only take rapid shallow breaths.
I’ve heard that when someone is crucified they die of asphyxiation. Hanging with your arms up in the air like that makes it difficult or impossible to breathe. After this experience I have no doubt that this is possible. Like I said, I wasn’t in any real danger. However it was extremely scary and frustrating to be in such a helpless situation. The new protocol for me sitting on the toilet is that dad or my caregiver checks on me every five minutes. 
Note: Not too long after that, I gave up using the lift to sit on the toilet and I’ve used a bedpan exclusively since then.
The rest of the day went really well. I went to see the new “Captain America: Civil War” movie with my friends Rich and Kathy. It was the first time they had taken me anywhere in my new wheelchair and my new van. That all went really well. Of course it was a little awkward not having done it before but it all went okay. I thought it was one of the best comic book action movies I’ve ever seen.
The Date is Set
On Tuesday, May 17 I had my appointment with the gastroenterologist. After the initial shock that we really were going to do the G-tube, in the days leading up to this appointment found a sense of relief. It had been so difficult for me to eat that the idea that I wasn’t going to have to struggle to do so anymore had somehow overridden any worries or dread that I had about the procedure itself. It seemed strange to be looking forward to a surgical procedure which I had been avoiding for almost 20 years. 
I have never been to this doctor before. His name is Dr. Mazen Alsatie. He’s a very likable guy who tended to joke around a lot which puts you at ease. I had had another gastroenterologist one time I referred to as “my asshole doctor” not because of his specialty but because of his terrible bedside manner. I was glad that this new doctor was much nicer.
I explained to him the difficulty that we could probably not get an endoscope down my throat. The normal procedure for putting in such a G-tube is a put a scope down your throat into your stomach and then that guides them were to poke a hole that your abdomen and into the stomach. Also expressed my concerns about general anesthetic which can be dangerous for me. He said he needed to talk to another doctor about my case and he would be right back “If I’m not back in a few hours, check with the nurse… Just kidding. I will be back in a minute.” Like I said he is a jokester.
He did return in just a few minutes. The plan that he came up with was to have a radiologist do the procedure outpatient at St. Vincent. I would have to drink some barium the night before. He even suggested I might go to the hospital the night before and they would give me the barium using a nasogastric tube. This is a tube that they stick up your nose and then down into your throat and into your stomach. It can be used temporarily for feeding or anything else they need to put in your stomach like barium for a procedure. We got a call the next day from the radiology department at St. Vincent and I set up my appointment for 10:30 AM on Thursday, May 26 which was just a little over a week away. We concluded that I could drink the barium normally so I would not need to go into the hospital the day before. At least that was the plan at that point. Things would soon change.
I spent the next several days trying to negotiate the copyright lawsuit unsuccessfully. Let me rephrase that… I wasn’t trying to negotiate unsuccessfully. I was trying to negotiate… However I was unsuccessful. On Friday, May 20 I got a visit from my friend and former caregiver Rick Ruiz. He had not seen my new wheelchair and it was fun to get caught up with him. While he was here that afternoon I started noticing some pain in my bladder. After he left I tried calling my urologist and ended up leaving a message on the nurse’s voicemail. It was about 3:30 or 4 o’clock so I wasn’t very hopeful that I would hear back from them. 
The next morning when I had not heard anything, I decided I should go to the immediate care center over in Speedway to see if they could get me an antibiotic. It’s a nice little facility at the end of Main Street. It’s normally very easy to get to however this happened to be opening day of qualifying for the 500. We decided to go a little bit of the back way and went on the highway to 10th Street and then back to Speedway. As it turned out there wasn’t any traffic there but it was still a good idea to long way around. We got in quickly and I met with a nurse practitioner and explained that I had recurring infections. I had brought a sample for them to test and it looked very nasty. I told her that my urologist usually gives me Levaquin 500 mg. It made her job easy because I knew exactly what was wrong and what I needed to fix it. I told her it reminded me of the time my mother took my sister Carol to the doctor when she was about five or six years old. Carol said “Mommy why do we have to go to the doctor if you already know what’s wrong with me.” My mom said “They won’t let me write prescriptions.”
The next day on Sunday I felt worse. I had a rough night Saturday night and slept in till afternoon. I just sat around and watched the second day of qualifying for the 500 on TV.  I began to get concerned because I had not been eating well that this infection was hitting me harder than usual. I told dad early Monday morning that I thought maybe we need to go to the hospital sometime that day. The problem was that dad had been suffering with a nasty case of shingles for several weeks. He had finally gotten a doctor’s appointment for Monday and I hated to see him miss it. I told him he should go ahead and keep his doctor’s appointment and then we would go to the hospital afterwards. Meanwhile that morning the urology nurse finally returned our call. Dad told her I was doing worse and was thinking about going to the hospital. She said since I was getting worse that was probably a good idea.
I began to get concerned because I had not been eating well that this infection was hitting me harder than usual. I told dad early Monday morning that I thought maybe we need to go to the hospital sometime that day. The problem was that dad had been suffering with a nasty case of shingles for several weeks. He had finally gotten a doctor’s appointment for Monday and I hated to see him miss it. I told him he should go ahead and keep his doctor’s appointment and then we would go to the hospital afterwards. Meanwhile that morning the urology nurse finally returned our call. Dad told her I was doing worse and was thinking about going to the hospital. She said since I was getting worse that was probably a good idea. 
Monday, May 23 I rode with dad to his doctor’s appointment and then we went on to St. Vincent. We got to the hospital about 3 PM. I gave them a urine sample and they drew blood and hooked up an IV. Of course you spend forever waiting on things in the ER. I managed to connect to St. Vincent’s free Wi-Fi while waiting in the ER. You could not get a cell signal but at least you could get Wi-Fi. I posted a quick message on Facebook.  It was several hours until we knew what was going on. They concluded that the infection had not gone systemic. That was one of my main concerns. Because I had not been eating very well I didn’t know what was going to happen with this infection. They decided it was best to admit me which is what I really wanted at that point. It was after 9 PM when they finally got me to a room.
It was several hours until we knew what was going on. They concluded that the infection had not gone systemic. That was one of my main concerns. Because I had not been eating very well I didn’t know what was going to happen with this infection. They decided it was best to admit me which is what I really wanted at that point. It was after 9 PM when they finally got me to a room.
We had a little bit of a logistics problem getting me to the room from the ER. When dad goes somewhere where he has to walk long distances, he needs to take his little three wheeled gogo scooter that we bought for mom years ago. So we had me on a gurney, dad in the gogo scooter, and my empty wheelchair all needing to go from the ER to the fifth floor. The nurse requested 2 people from transport to assist with moving my wheelchair. But somehow the message got mangled. They sent one guy to push the gurney and then another guy came along with an empty push wheelchair. When he saw the first guy taking me on the gurney he thought they didn’t need him.
I wasn’t really anxious to have the wheelchair itself. I would not need it for many days. But sitting in the wheelchair was the bag containing my CPAP machine and also my special call button. For those of you who have read stories of some of my previous hospital visits, you know that I have a little push button on the end of a wire was made for me by the rehab engineering people at St. Vincent perhaps 30 years ago. I just take it with me anytime I need to go to the hospital. It plugs into their call system and it has a really light touch that I can use. Dad didn’t want to leave until I had the call system set up and was all settled in. Eventually the nurse from the ER who had been taking care of me brought the wheelchair up herself. I guess if you want something done right you do have to do it yourself.
We plugged in the call button and set up my CPAP machine. Dad didn’t get to leave until about 9:30 or 10 PM.
Too Many Damn Rules
Dad and I have a running joke whose punchline is “There are too many damn rules”. It usually comes up when we are watching a football game and the referee calls some really obscure penalty. Dad always says “There are too many damn rules.” He wants to just let them play the damn game. We quote that line and are so many other circumstances that it has got to be a cliché. Who knew that I would run into it at the hospital that night.
When you use a CPAP machine that you bring from home, it is supposed to be checked out and set up by someone from respiratory therapy. The therapist had stopped by just minutes after I arrived in my room. At that point the CPAP was still with the wheelchair down at the ER department. When the wheelchair finally arrived, the RN who was assigned to me went ahead and set up the CPAP and put it on me.
I explained to him that I needed a humidifier in the oxygen line. The way it works is that there is a receptacle in the wall that feeds out oxygen. You put a little container full of water in that line and the oxygen bubbles through the water to human it. The oxygen line then plugs into the hose on the CPAP to provide humidified oxygen in addition to the pressurized room air that the CPAP provides. That’s the way I’ve done it for years at home. When I first started on CPAP 30 years ago, the humidifiers that you would use with a CPAP were not very reliable. You could not control the amount of humidity. Even though newer CPAP machines have sophisticated temperature and humidity controls, when I replaced my machine several years ago they offered me a heater/humidifier but I didn’t think I needed it. My nurse, a really nice guy named Pete, had no problem hooking up the bubbler in the oxygen line connecting everything like I wanted.
Then about midnight the gal from respiratory therapy returned and looked at the CPAP set up. She said we could not have the bubbler in the oxygen line. She said that there was a risk that the back pressure from the CPAP could cause the bubbler to explode. She wasn’t just talking about it springing a leak and squirting water. She said something to the effect of “we don’t want anyone getting hurt” as if it was going to shower the room with shrapnel. The whole idea was totally ridiculous. Yet she insisted that it was a firm “hospital policy” with no room for negotiation. So she removed the bubbler and connected the oxygen line directly into the CPAP with no humidification. I figured I would be okay. Sometimes my humidifier at home dries out and I don’t notice it for a day or two.
My decision to go ahead and use the oxygen without the humidifier would come back to haunt me later. The respiratory therapist I had for the second night came up with another silly rule. I had to have an oxygen meter connected to my finger anytime I had my CPAP on. She wrapped it around my finger so tight that it made my finger throb. I eventually got the nurse to loosen it up to where it was comfortable. The irony is if I have on my oxygen and my CPAP my oxygen level is always usually in the high 90s. It’s more likely that I would need the oxygen meter when the CPAP was off but they don’t care about that. The rule is you only need it when your oxygen is on. Fortunately I only had to do that one night. None of the other respiratory people seem to care about it the rest of the week.
There are too many damn rules.
Staying Connected
I had a reasonably comfortable night in the hospital the first night. The following morning, dad had an appointment of his own. In addition to his problems with shingles, the also was concerned he was having some gallbladder problems. The doctor scheduled him for an ultrasound on the morning of Tuesday, May 24. He had that procedure and then came to the hospital to visit me. He brought my laptop and I was able to get online. It also gave me the opportunity to catch up on some TV shows that I had downloaded and some YouTube videos I wanted to watch. And of course it gave me the opportunity to keep in touch with everyone by Facebook. 
Not only does my laptop give me access to the Internet and anything that I might have stored on the laptop, I can use Team Viewer remote access software to log into my desktop at home and get access to anything on that machine. While most people use some sort of webmail to access their email, I’m kind of old-fashioned and I use Microsoft Outlook and a POP3 access to download all of my email to my desktop machine. The disadvantage is that if Outlook is running on my PC and captures the email, there’s no way to access it from a webpage. I had deliberately left my desktop running but forgot to mention to my dad that it was intentional. He had shut it down when he got home. While that meant I could not access my desktop computer, it also meant that Outlook wasn’t running so if I accessed webmail then unread emails would still be there. I was anxious to see if there was email from my lawyer. The guy who was suing me for copyright infringement had said that he was going to file the lawsuit either Monday the 23rd or Tuesday the 24th depending on which threatening email you believed. I was able to contact my lawyer by webmail and tell him I was in the hospital. He said that my opponent had filed several lawsuits on Monday but mine was not among them. It turned out that he did not file the suit until a couple of weeks later.
Input and Output
You see a number of doctors over the course of the day. There is generally an intern or resident who is directly assigned to you. He or she then reports to the chief resident and in turn they both report to an attending physician. They all confirmed that I was doing well. The infection had not spread and they seem confident that while I was still in the hospital we could proceed with the G-tube procedure perhaps as soon as Wednesday the 25th. 
I was concerned that I wasn’t urinating very much however they said that my blood work indicated that my kidneys were functioning okay. With the IV constantly running I expected to be putting out more fluid from the other end. I don’t know where it was going but we were certainly putting in more than was coming out.
At one point they sent in a nice young woman who was from the speech therapy department. Her actual goal however was to investigate how well I could swallow. I gave her my complete history of swallowing. She had me tried to swallow ice chips, applesauce, and to drink water. She came to a conclusion that I had already known for a long time. I can’t swallow worth a damn. Her recommendation ended up being that I have absolutely nothing by mouth. Although I didn’t necessarily agree that I could have nothing by mouth, it meant that I would not have to drink the barium. Drinking barium is a nasty business even when you can swallow well. The more I thought about it, the more I liked the idea of using a nasogastric tube. So the good part about her conclusions were that we were definitely getting the NG tube. The plan was that they would put it in about 10 PM Tuesday night and give me the barium. The G-tube procedure would be Wednesday morning.
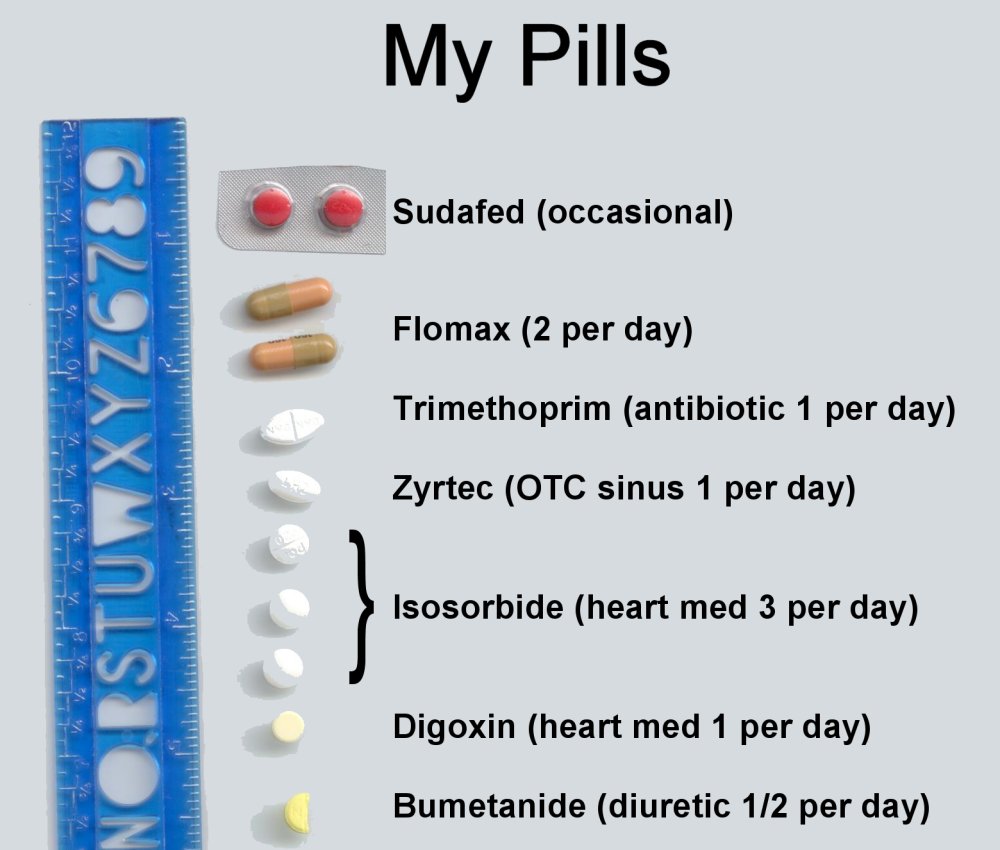
One of the other issues that concerned me was I wasn’t getting my normal medication. I was getting y digoxin heart medication and my Flomax. But I was not getting my isosorbide which is a heart medication I take three times a day nor was I getting bumetanide which is a mild diuretic. They said the reason was that my blomod pressure was a bit low and that you should not have either of those with low blood pressure. Usually my blood pressure is a typical 120/80 or thereabouts. They were getting top numbers barely above 100/70 something.
There was also an attempt on several occasions to give me some sort of injection that was a blood thinner. They said they were worried about blood clots. I guess it would’ve been from lying around in bed. I tried to explain to them I was going to have a G-tube surgical procedure very soon. I didn’t want to show up in surgery and have the surgeon all of a sudden notice I had been getting blood thinner and say “What the hell I can’t do this if he’s on blood thinner!” Every time I refused the blood thinner shots, I asked them to verify if it was okay to take the shot given that I’m scheduled for minor surgery in the next day or two. I never did get a reply. But they did not give me the shot so I didn’t worry about it. Even after the G-tube was inserted a couple of days later, they still wanted to give me the blood thinner. I continued to refuse because I knew in a day or two I was going to be putting on my back brace. The way it digs into me in various places I would’ve been a bruised up mess.
Names and Accents
Tuesday evening after the shift change I was pleased to see I had the same nurse that I had the first night. I said to him “Yesterday you said your name was Pete. Today I’m going to call you ‘Re-Pete'”. I also told a number of the other nurses the same joke. They all liked it. Unfortunately Pete had some bad news for me. We were not going to do the NG tube Tuesday night because we were not going to do the G-tube Wednesday morning. Somehow I had been misinformed and it was all pushed back to do the procedure on Thursday at my originally scheduled time.  Other than the disappointment that everything was still pushed back until Thursday, my second night was uneventful.
Other than the disappointment that everything was still pushed back until Thursday, my second night was uneventful.
The morning of Wednesday, May 25 I was visited by the usual parade of doctors starting with the early year resident, followed by the chief resident and eventually the attending. My attending was a woman named Dr. Maryam Massoumi. She is sort of an exotic looking woman with a fascinating accent that reminds me a great deal of one of my favorite actresses Shohreh Aghdashloo. I never have been able to pronounce the actress’s name. The first time I saw her was when she played a terrorist in season 4 of the TV series “24“. Mostly my doctor sounded like the actress but she actually resembled her a little bit. You can click on the links of their name to see photos and biographies of them. The actress always plays parts where she’s doing something sneaky. Most recently she has played a politician in the sci-fi series “The Expanse” where she is very sneaky. Her sultry voice makes you believe whenever she’s saying. That same voice coming from your doctor has a rather soothing effect. I got so interested in her accent that I eventually later in the week asked her where she was from. It sounded Iranian or Persian (approximately the same thing) which is where the actress is from. However I didn’t want to say to her “Hey are you Iranian?” and then it turns out she is from some other Middle Eastern country that is a mortal enemy of Iran.
It was late in the week when I finally figured out a way to inquire. I told her outright that her accent had a soothing quality to it and I wondered what kind of accent it was. She said it was Persian and I successfully suppressed my urge to shout “YES! I nailed it!” I do think I probably said something like “I thought perhaps that was it.” She said she had spent lots of time in Brussels. If I had thought to Google her or look her up on the St. Vincent physician directory I would’ve seen where it says “Languages: English, French, Farsi.” In case you haven’t watched enough movies or TV shows about the Middle East, Farsi is spoken in Iran.
She said that she was concerned that my infection might not be entirely confined to my urinary tract. She wanted to do a chest x-ray just to make sure I did not have some sort of pneumonia hiding out. I had been told that after they put in the NG tube, they would need to do an x-ray to make sure that it was in the proper place. I suggested we save the trouble of two x-rays, put in the NG tube, and then do one x-ray for both. She agreed. It turned out that was a good idea for more than one reason. I wasn’t scheduled to get the NG tube until about 10 PM that night however to double up the x-rays we went ahead and tried to put the NG tube in the morning. We had difficulty getting the NG tube in and it took several attempts. If we had waited until that night we might not have got it done it all. 
Pushing Your Limits
I’m sorry I don’t remember the name of my daytime nurse but she was really nice and did a good job. She tried to insert the NG tube three different times but it just wouldn’t go. One of the problems is that they thought I needed to be sitting upright in the hospital bed as high as I could go. I’m not used to sitting up without my back brace on. It makes me very slumped without the brace supporting me and that also makes it difficult to breathe sometimes. Naturally you’re going to gag if they stick a tube up your nose and down your throat. But I got pretty messed up and ended up sucking some saliva into my lungs. We had to give up after three tries. 
Shortly after that, the girl arrived with the portable x-ray machine. We went ahead and did the chest x-ray even though we did not yet have the NG tube in place. X-ray machines these days do not use x-ray film. They are all digital. They have a large metal and plastic plate which looks like the plate that they used to use to hold the x-ray film. I don’t know if it has sensors built into it or if somehow it reflects the x-rays back towards the machine or how it works exactly. There’s no cable running from the plate to the x-ray machine so if it is a sensor not a reflector it must be wirelessly connected.
Again they wanted me to sit upright as straight as I could. She raised the bed as high as I could stand it. I did not think about the fact that then we needed to jam the plate behind me. I had already leaned forward as far as I could and then I had to go further still. Dad was there and he helped her stuff it behind my back. That was uncomfortable but not as bad as when they tried to take the plate out. As they leaned me forward to pull it out, I strained a muscle in my ribs on the left side. I don’t think I cracked a rib but I came awfully close to doing so. If I had done it on the way in, the x-ray would show whether or not I cracked a rib. But the sprain came as they were taking it out.
Fourth Time is the Charm
After our three failed attempts to get the NG tube up my nose and down my throat they said they were going to send up someone from radiology to attempt to do it. However there was another nurse across the hall who had more experience and she agreed to give it a try. This time we did not sit me up as straight. Given my sore ribs I didn’t think I could take it. She also used a slightly smaller tube than the previous nurse had used. While it was very uncomfortable and I did gag a lot, we ended up getting it down okay. I told the other nurse that she had no shame in her three failed attempts. The other nurse was cheating using a smaller tube and having me lie down where I was more comfortable. The truth is I think perhaps the first nurse did actually have it most of the way in during one or more of her attempts. But I was gagging so hard and aspirating saliva that it felt like it was in the wrong place. I think if she had gone ahead and I was able to cough up some spit we would’ve been okay. 
After we had the tube in, they had to bring back the x-ray machine to do a second x-ray and see if it was in the proper place. I asked if they could do it with me lying flat rather than sitting up and they agreed. It turns out the NG tube was okay. Also the previous x-ray showed no problems with my lungs so that was good news.
I had hoped that once we had the barium in me, we would be able to remove the NG tube. Unfortunately that was not the case. They had a very good reason for wanting to leave it in. During the procedure of putting in the G-tube in my stomach, they wanted to use the NG tube to blow my stomach up full of air. That would push it forward against my abdomen wall. Then they can poke a hole into me through the abdomen and directly into the stomach.
Leaving the NG tube in was going to complicate things overnight. The mask on my CPAP uses a system called “nasal pillows”. They are the rubber things that stick into your nose about 3/8 of an inch. I wasn’t sure that I would be able to get the CPAP mask on my nose with the NG tube sticking out my left nostril. I laid there thinking about different ways we might do it. I thought maybe we could plug up my nostril that had the NG tube and tape over half of the CPAP mask just have it blow in one side of my nose.
While waiting for 10 PM to roll around, I tried to take a nap but without the CPAP on I kept having apnea attacks about every 60 to 90 seconds so I really didn’t get any rest. When we put the barium in at 10 PM it all went very smoothly. We got the respiratory therapist to come down and try to put the mask on me. They had taped the NG tube to the front of my nostril but we removed the tape and repositioned it off to the side. We then put the mask on and it did fairly well. It was leaking quite a bit but the CPAP has built-in sensors to maintain the proper air pressure even if there are leaks in the system. The leaks were not so distracting that I could not sleep with it. It went pretty well throughout the night. 
Last-Minute Setback Averted
It’s Thursday morning May 26 and it’s the day to have the G-tube procedure. I wanted to leave my CPAP on as long as possible so that I was well rested and fresh for the procedure. My original appointment was for 10 AM in outpatient but that was my arrival time. I later learned that the actual time for the procedure was supposed to be about noon. However they later came in and said it had been pushed to 2 PM. At one point I tried taking the CPAP off and I had a real problem breathing without it. The combination of the irritation of the NG tube and spending three nights without humidified oxygen had messed up my throat really bad. Every time I tried to breathe it felt like my throat was closing up. I got really worried because I didn’t think I would be able to take the CPAP with me during the procedure. If I could not find a way to wean myself off of it by the time of the procedure, we would have to cancel.
After about five minutes with the CPAP off I had to have them put it back on me again. Shortly thereafter dad arrived. I kept doing experiments when I would try breathing through my mouth without using the pressure of the CPAP. Over the course of the rest of the morning I gradually started breathing a little easier. It was a good thing that they had pushed the procedure to 2 PM instead of the original 12 noon start time. I needed that time to get my lungs going again. I had told the nurse I was having difficulty getting off of the CPAP. She set up a regular oxygen nasal cannula for me to use oxygen when I took off the CPAP.
Sometime around 1 PM I was able to switch from the CPAP to the straight oxygen. One of the things that helped was that someone from respiratory therapy department came down for a visit. She agreed to let me use the humidifier in the oxygen line. More on that story later. I think the humidity and just getting wider awake and swallowing a little bit got my throat in better shape. I was able to keep the nasal cannula oxygen on during the trip to the procedure and throughout the procedure and the way back afterwards. By the time it was all over with I was breathing normally but it was nice to have the oxygen just in case.
Time for Surgery
They eventually came to get me at about 1:30 PM. Dad was able to go down with me. They rolled me into a pre-op area and the doctor who was going to do the procedure came out and had a conversation with us. He did a great job of explaining everything that he was going to do.
One of the questions I had had from the beginning was “How do you get the stomach to stick to the abdomen wall once you get the tube in. He explained that there would actually be a couple of stitches. He said they were like little plastic T-shaped gadgets that holds tags on to clothing when you first purchase it. With dad and I being more familiar with construction then retail clothing, we said “You mean like a Molly bolt”. He explained that the stitches would come out after 10-14 days. I asked him if a visiting nurse could do it. Perhaps the nurse from Acme Homecare could remove them. I knew I would need to be recertified before my home health aide could return and I would be getting a visit from their nurse. He said possibly yes. I would also need to follow up with my regular doctor and he might be able to do it.
He explained that the reason for the barium was so they could see where your transverse colon is. They have to make sure it’s out of the way. I told him that I had previously had 12 inches taken out of my descending colon and that that probably repositioned where my transverse colon was. He said that they would inject my abdomen with local aesthetic and I would not feel a thing. I told him my old standing joke where I used to think that “local anesthetic” meant that it was produced here in Indianapolis by Eli Lilly.
He said that they would give me a mild sedative to keep me calm. I told him I wanted the absolute minimum because I was concerned about my breathing. I explained that if something happened in an emergency they would not be able to intubate me in my mouth because my mouth doesn’t open. I explained anytime I was intubated they had to do it through the nose. He said that he was going to give me Versed which is a type of anesthetic that makes you forget. After the procedure was over I am 99.9% sure that I remember all of it. There was a running conversation throughout it and I don’t remember any gaps. But then again if it is supposed to make you forget, who knows when I missed. I only recall feeling the tiniest bit groggy.
He told my dad that the procedure would only take 15-20 minutes but by the time they rolled you into the operating room, get you transferred to the table, shave your hairy chest, drape you, get all of the equipment in place it actually took a little more than twice that. I told them that I recalled being in an OR that was this one or one just like it before. When I had been in the hospital for my bowel resection, they had to put a central line into my juggler and had used x-ray assistance to do so. They told me there were actually 4 rooms just like this one and I would have been in one of them for such a procedure.
The procedure itself was painless. I felt a tiny little stick of the needle for the first shot of lidocaine. Sort of like in the dentist when you feel the first shot but none of the others. Apparently my intestines were already pushed out of the way so they had no trouble getting to my stomach and getting it blown up into the proper position. You can feel the pressure when he would poke holes into me but it didn’t hurt. Also after everything had worn off I did not have any pain whatsoever. 
They rolled me back out to the waiting area and went to get dad. He was a little bit concerned about the length of time but I explained to him the procedure itself did indeed take about 15 minutes but it was all the stuff getting ready that took the extra time. Because I really hadn’t been sedated, they didn’t need me to stick around for “recovery time” like you would after some surgeries. They wanted to take me for an ultrasound after the procedure. I suggested to dad that he should go get something to eat and meet me back at the room later.
I seem to have lots of bad luck with the transport people. The first evening we couldn’t get anyone to bring my wheelchair up from the ER. The guy who was going to take me to the ultrasound lab instead took me to MRI. He delivered me to their waiting area and handed them my chart. I had seen the signs on the wall saying it was MRI but I figured perhaps they shared a common holding area. He was gone less than five minutes when he returned and said “I took you to the wrong place.” I eventually got to the ultrasound place okay.
The guy who did the ultrasound was really nice. The way I was laying I could see the screen and so I asked him some questions along the way. He pointed out my stomach, liver, kidneys, etc. We also talked about other things. I don’t know how the conversation got around to gambling. Perhaps we had started talking about sports and from there I said that I occasionally bet NFL games. It turns out this guy uses the same gambling websites that I use for poker and sports. I said to him “Either you have a really good poker face or you didn’t see anything shocking. At no time did you suddenly gasp and say ‘my God look at that!'” He said he didn’t really see anything except of course that my insides are kind of rearranged and that I have an enormous bladder which I had already told him to watch out for. He said there was a tiny bit of fluid loose in my abdomen but it wasn’t anything to worry about. I’ve always wondered if there wasn’t something extra sloshing around inside me so I wasn’t surprised. I could write a whole blog on that topic.
When I returned to my room I got online and posted a brief newsflash on Facebook saying that the procedure was over and went well. Then I posted a follow-up with more details. By the way they did take out the NG tube once the procedure was over with. I don’t recall if they took it out in the radiology department or if I got it out when I returned to my room. But it was a relief to be free of that. 
Not so Many Rules after All
I mentioned that just prior to going for my procedure, a respiratory therapist dropped by and put the bubbler in my oxygen line. I said there was more to that story so here goes…
Somewhere around Tuesday or Wednesday I was visited by a nursing supervisor who asked if I had any complaints about the care I was getting. I told her that all the people had been really great. She specifically asked if anyone stood out and I told her that Pete/Repeat was an especially nice guy but everyone had been wonderful. As a last thought, I said to her “I’m generally not a complainer but since you asked my opinion… I do have one bit of a complaint.” I told her the story about the respiratory therapist who said that “hospital policy” was that you could not have a bubbler in your oxygen when used with a CPAP. I speculated with her as I had done every time I told the story. Probably someone had their CPAP cranked up too high, the little plastic bubble bottle was defective, it popped open, the lawyers got involved, and now we have a stupid rule. She took note of everything that I said. She was unaware of such a policy.
Now on Thursday just before I went to my procedure, I was visited by the respiratory therapist. She asked me about the humidifier bubbler and I told her the whole story. She said that she had never heard of such a policy. She put the bubbler in after getting permission from her supervisor. A little bit later in the day, that supervisor stopped by and talked to me about it. She too had never heard of such a policy and she was a supervisor! I told her that I had talked to the nursing supervisor about it even though I don’t generally raise a fuss. The respiratory supervisor said that the nursing supervisor had sent out an email that had gone up and down the chain of command and gone to her own supervisor. That is the daytime respiratory therapy supervisor got email from her boss about this so-called policy that in fact did not exist.
I told her that this had occurred Monday night at about midnight. I did not get the name of the person that told me about this inflexible hospital policy. The supervisor told me she would talk to the night supervisor and try to figure out who had been on duty that evening and where these crazy ideas came from. I never did hear any more about it but it was kind of rewarding to think that somebody was going to get called in on the carpet and get a talk about making up rules. Perhaps she worked previously at a different hospital that had such a rule. Who knows.
I said throughout I don’t like to complain. Actually I do like to complain but I don’t like to raise a big stink if I don’t think there’s any chance of it doing any good. I did a lot of complaining to the nurses, on Facebook, friends and family. I just figured I was up against an entire hospital bureaucracy and wasn’t going to get any relief. I was wrong. I’m glad the nursing supervisor asked my opinion because I do like giving opinions :-). For once, speaking up against bureaucracy turned out to get results after all. 
Tube Me, or Not Tube Me?
I will give you a “TMI” (too much information) warning at this point. If you don’t like to read about the somewhat personal, gross stuff you might want to skip this section.
One of my big concerns throughout the hospital stay was that I did not seem to be urinating very much despite the fact that I had an IV of saline, D5, and antibiotics running 24/7. At one point they also noticed my potassium was too low. Giving you potassium by IV is always tricky because it burns your veins going in. If they can get it diluted with other IV stuff it’s not too bad but if they have to give you a lot of it, it can be quite painful. Anyway it seemed to me and everyone else that they were putting lots of fluid into me but not much was coming out.
At one point they did an in-and-out catheter and got over 1000 mL of urine. From time to time they would do an ultrasound on my bladder that would measure the volume of liquid. One time in the hospital previously they noted that I had 700 mL and I didn’t even feel a tiny bit full. Throughout this experience it was common for them to measure 800 or 900. They told that a normal person would feel like they were ready to explode at 900. I barely felt anything at that level.
After they took the 1000 out, it took a long time for my bladder to fill up again. They kept measuring it with the scanner and it would gradually increase. But I never felt like I had to go much. Somewhere along the way they finally called in a urologist. Up until that time I had been treated by internal medicine doctors and not specifically urologists. Sometime on Friday, the day after the G-tube procedure, they tried another in-and-out catheterization but it would not go in.
In addition to my severe scoliosis (curvature of my spine) both of my hips have been dislocated for many years. In fact one x-ray revealed the ball part of the ball and socket of one of my hips has been grinding in my pelvis for so long that it has ground itself a new socket. That was in x-ray maybe 20 or 30 years ago. God knows what kind of mess my hips are in at this point. So that, combined with my freakishly large bladder means my internal anatomy is pretty messed up. The path into my bladder has a lot of curves and makes it difficult to put in a catheter.
In addition to the urinary issues, when you pump strong antibiotics into you over a long period of time, diarrhea is a natural side effect. You end up killing all the good digestive bacteria along with the bad stuff. For the last couple of days of my hospital stay I was extremely, extremely loose. Fortunately I was always able to get on the bedpan in time.
At one point the urologists called for a cart to be sent from the O.R. that they described as “cysto-to-go”. It sounds like the name of a fast food restaurant for urologists 🙂 Basically it’s just a portable cart with a urinary cystoscope and everything you would need to go with it. I was visited by a pair of nurse practitioners from urology and I talked them out of the idea of anchoring a Foley catheter. That was early on Friday. However late Friday evening a urologist who is one of the partners of my usual urologist came in. He talked me into going ahead and putting in the Foley since he wanted to do it using the scope. I told him about the difficulty my regular urologist has always had catheterizing me. He usually does it using a guidewire. Anyway late Friday night he brought in the cysto-to-go and did the procedure. It went reasonably well and it was good to know I was going to be really empty for the rest of my stay in the hospital. I probably should have let them do it sooner.
It’s now safe to continue reading if you want to avoid the gross stuff.
Tools and Talent Is All It Takes
After the G-tube procedure, they had attached a low-power suction tube onto it to make sure there wasn’t any drainage or bleeding. On Friday, the day after the procedure, they disconnected the suction and started pumping nutrition using a continuous feed pump. Throughout that day they gradually increased the rate and if that went okay (which it did) they would start doing what is called a bolus feeding they have a large syringe of about 60 or 70 cc and just pump it in by hand. 
They were talking like I could go home Saturday or Sunday. Saturday would’ve been okay but Sunday would’ve been tough because it was race day. The only time you can get in or out of my neighborhood on race day is during the race itself. If you’ve ever been in the hospital, you know that they never release you on any particular schedule. There’s always some last-minute form that needs to be signed or an IV that needs to be removed but the nurse is too busy to do it. Even if dad could get to me, the idea that we would get released and arrive home during the race was really unrealistic. Also because the race was sold out for the first time in decades, they were going to allow it to be shown live on local TV. I didn’t want to have to watch it recorded on the DVR because I was traveling during the race.
Before I can think about going home, we had to do some work on my back brace. Now that the G-tube was in place and there was no suction connected to it, we could experiment with putting the brace on me and decide where to cut the hole. Dad had brought a tape measure and a battery-powered drill. The drill have a large drill bit about an inch and a half in diameter. It’s the kind of drill bit that you would use to cut a hole for a doorknob. The one thing we didn’t have was a marking pen to mark the spot to drill. But we borrowed one from a nurse.
My back brace is in 2 sections, a front and a back piece. We slipped the back piece underneath me and then measured from each side how far it was left or right to the G-tube. Because we were measuring across my belly which was going to be inside the brace, the overall distance was slightly less than what it would’ve been with the front half of the brace on top of me. We needed to get the ratio of distances left or right and then measure the entire distance on the outside of the front half of the brace. As it turned out the tube was going to land within a half inch of dead center so there really wasn’t much math involved. And the distance across my chest was only about a half inch less than the outside measurement across the front of the brace.
The hole that we were going to cut would have to be a vertical slot about an inch and a half wide and maybe 3 or 4 inches tall. We start out with the brace on me very low. Throughout the day I gradually slip down inside of it and the brace rides up. So throughout the day the hole would move up relative to the G-tube. Dad took all of the measurements, got in his go-go scooter, went down to the van in the parking lot and cut the hole. When he brought it back it looked as though it was going to work perfectly.
The Mystery Pain Returns
On a few occasions over the years, I have gotten some mystery pains around my back in the shoulder blade area and in my chest around my ribs. It is an area where the top edge of my back brace puts the most pressure on me. It doesn’t hurt much during the day when the brace is on. It doesn’t hurt when I take the brace off. It only hurts hours later in the middle of the night. It feels like a cross between muscle cramps and a burning sensation sort of like heartburn. Most of the time when I’ve had it, it wasn’t too bad and it just went away. Probably my most memorable episode was in 2006 when I was in the hospital having intestinal surgery when my intestines ruptured. It was several days into the ordeal and I had pain that felt like heartburn. For various reasons they couldn’t give me Rolaids or Tums without specific doctor’s orders. But they already had orders that I could have morphine because of my surgery pain. So I had them give me a shot of morphine instead of an antacid. Here’s a link to a previous blog post about that.
Rolaids vs. Morphine
There was another incident in 2014 when I woke up in the middle of the night with pretty bad chest pain. Although it did have a bit of a burning sensation associated with it, this felt more like real chest pain and it was very bad. I tried calling dad but for some reason he was sleeping especially sound and I couldn’t wake him up. After about a half hour the pain went away. If it had persisted and/or I had gotten him awake I would’ve called 911. A week or two later I had it again in the middle of the night and although it let up for a while, by morning it was back again and pretty bad. This was May 1, 2014.  On that occasion I did end up going to the hospital in an ambulance. They checked all of my cardiac enzymes and EKG etc. and said there was nothing wrong. I spent one night in the hospital and went home the next day.
On that occasion I did end up going to the hospital in an ambulance. They checked all of my cardiac enzymes and EKG etc. and said there was nothing wrong. I spent one night in the hospital and went home the next day.
Unfortunately I’m one of those people who watches too many medical TV shows. On several shows I’ve seen them talk about something called “crush syndrome”. It’s whenever they rescue someone at a collapsed building or someone who got buried in wet concrete that solidified too quickly and stuff like that. They say that the pressure on the person’s body causes toxins to be built up in the tissue and then when they relieve the pressure and the blood flow returns, all of those toxins come pouring out into the bloodstream and they can be really dangerous. It got me to thinking that perhaps the pressure of wearing this tight back brace all day long make something weird build up inside me and then when it finally cuts loose I get the burning pain. But if the TV shows are accurate, there’s always a race against time to quickly give the patient whatever they need to get rid of the toxic stuff immediately. My painful situation is always delayed hours after taking my brace off. My situation doesn’t really line up with the sort of emergency depicted on TV.
Because I have had one of my biggest instances of this particular pain while in the hospital to begin with, I’ve often wondered if it was because I was missing some of my regular medication. One medication I routinely miss while in the hospital is the daily dose of Zyrtec antihistamine. Even though it’s an over-the-counter medicine it’s probably only to be used “as needed” but my sinuses are such a disaster area that I take one every day religiously. I also use at least one sometimes two different kinds of nasal steroids. Maybe there such a thing as Zyrtec withdrawal. Perhaps I am getting some sort of minor version of crush syndrome but the Zyrtec counteracts it.
So anyway enough of the history of my weird chest pains, Friday night May 27 in the middle of the night, I started getting those familiar weird pains. In addition to not having any Zyrtec for several days, I had also been missing my isosorbide which is often prescribed for angina (i.e. chest pain). I don’t recall missing taking any isosorbide on previous occasions where I’ve had the pain. Anyway I asked the nurse for some Tylenol and he took some pills and crushed them up in a pill crushing gadget. He dissolved them in water and put them into my G-tube.
The Tylenol didn’t seem to help at all and if anything the pain was getting worse. On the proverbial scale of 1 to 10 it started out as a 2 or 3 and now was clearly up to about 5 and getting worse. This time I did not have standing orders for morphine. The nurse got in touch with whatever doctor was on call to try to get something stronger. They didn’t want to jump all the way to morphine so he prescribed a pill called Tramadol. Again they crushed it up in a pill crusher, dissolved it in water, and put it to the G-tube. After about 15 minutes I got this really warm rush feeling all over and the pain started to fade. This was about 7 AM. I posted on Facebook about four hours later that everything was okay. 
Note: I have since concluded that this recurring pain that I seem to get in the hospital and other times at home is likely from sitting up too straight in the hospital bed without my back brace on. My regular doctor has given me a prescription for Tramadol. I generally need it no more than about once a month. Tramadol notoriously makes people sleepy but for some reason it initially has the opposite effect on me. At home if I take it at bedtime it keeps me awake all night and then when it wears off I crash and get very sleepy. It’s strange that I never noticed I have lots of little aches and pains all the time that I typically ignore and when I take Tramadol they ALL go away. It cures me of things I didn’t know I had 🙂 I can see how someone could easily get addicted. I don’t think I really get high or catch a buzz but that relaxing feeling of all my aches and pains disappearing for a few hours sure is attractive. I’m trying to be careful not to abuse it and so far I’m succeeding. Like I said, I think maybe one per month.
My theory about so-called “crush syndrome” was fading rapidly. Although I did put my brace on earlier that day. It was only on me for about five minutes while my dad did a test fitting to figure out where to put the hole and then again to see that all was in the right place. I don’t believe we even tightened the brace all of the way and I did not even sit up with it on. Perhaps this particular pain was from the back strain when we did the x-ray. There had also been this week an incident where the nurses were sliding me up in the bed towards the head of the bed. You naturally slip down further into the bed whenever they raise your head up. They used to put something called a draw sheet completely underneath you. They could use it to yank you around. But for some reason the draw sheet was only beneath my rear end and part of my back. They needed the draw sheet to be clear up under my head and shoulders as well because I got kinked up pretty badly one time when they scooted me up. As I was describing all of this to a friend of mine several days later, she suggested that because it was a combination of muscle pain and a burning sensation perhaps it was a pinched nerve. I’m beginning to think that may be the thing. Although I didn’t have any more pain that Friday night/Saturday morning, it was the last incident of this particular problem.
Phenomenal Support
If you have happened to click on any of the Facebook links throughout this blog post, you have not only seen my thoughts in real time about the events I’m describing, so you have seen the tremendous number of well-wishers in the comments and even more “Likes” from friends, family, and even mild acquaintances who happen to be on my Facebook friends list. The prayer support was phenomenal.
It’s always been tradition that whenever I go to the hospital, I called my friend Margaret Arthur who is been in charge of the St. Gabriel prayer chain for as long as I could remember. If you have a prayer request, you give her a phone call and she calls 4 other leaders of the chain. They in turn each call one or two people who calls the next person and so on. I’m not sure how the chain is organized these days but at its height we had 30 or 40 people in the chain. Sadly Margaret passed away a couple of months ago. She was not only the “go to” person for prayer support, she was also a great source of information about everything that was going on in the parish. She would call me with frequent computer questions but in recent months her mind was not what it once was. Even when she was in good shape she was a little bit flaky 🙂 However she had to give up much of her volunteer work because she just wasn’t sharp enough to handle it anymore. I always knew what was going on in the parish, who was sick, who was in a nursing home, and who died. When I knew she was getting worse, I was worried that I would not know if she died because she was always my source of information about such things. Indeed when she did pass away, I did not hear about it until several days after the services.
I don’t know if we still have a telephone prayer chain but we do have a list of people that we pray for at mass each Sunday. At one point throughout the week (I forget when) I called St. Gabriel to let them know I was in the hospital. I had previously sent email to Fr. Mike looking for a time where he could anoint me prior to the G-tube procedure. I did not hear back from him right away and as it turned out I really didn’t think I needed to be anointed because I was not going to have general anesthetic. Not only was I feeling the loss of Margaret Arthur, I wasn’t really sure who would be answering the phone at St. Gabriel. Parishioners Linda Miller and Barb Williams had shared secretarial duties in the past but both of them had recently moved on to other things.
When I called St. Gabriel, the new receptionist reminded me of something I should’ve remembered. Fr. Mike was gone for a trip to Guatemala where we do missionary work at a sister parish down there. She said that he would be home for the weekend but would probably be very busy getting follow-up after his trip. I told her to go ahead and put me on the Sunday prayer list but that Fr. Mike did not need to visit unless he was already making rounds at the hospital. I would probably be home by the time he got around to it. After I returned home, I did get a visit from Fr. Mike even though I told him I was doing okay. It was nice to spend some time just chatting with him and to show him around my office with all of my computer equipment.
One sort of new person in my support system was a woman I have known for 40 years but had only recently reconnected with her through Facebook. Ellie Vinci was a dear friend from my college days. Although most of my time at IUPUI was spent at the 38th St. campus, I did spend one semester at the downtown campus and that’s where I met Ellie. I could probably do multiple blogs about my relationship with her but the short version is she was the first girl I ever went on a date with who was not in a wheelchair. She also took me to my first hockey game. Although she was normally a very mild-mannered and sensitive person, when she was at a hockey game she would scream and yell and curse like a sailor. I’ve often described her as a lovely sweet person who taught me a deep appreciation of violence on ice 🙂
Anyway… The week before I went in the hospital for some reason I decided to search for her on Facebook. We have talked several times off and on over the years. We have run into each other different places that we had not stayed in close contact. Just as we reconnected on Facebook, she said she was going on vacation with her two daughters to visit Rome and Sicily. With a name like Vinci you can expect she has connections to the region. In fact she traces her ancestry to Sicily. On one of our dates we had gone to see “The Godfather Part 2”. She said at the time “It’s about my people” although I don’t think she was claiming any actual Mafia connection… Just Sicilian connections.
While it I was in the hospital it was fun to watch all of the great photos she was posting on Facebook while in Rome. I told her to say hi to the Pope for me. She later posted that she had prayed for me at the tomb of St. Peter.
It wasn’t just Facebook friends or friends traveling in Rome that were supporting me. I also had a few visitors in the hospital. Our friend Jack Brake stopped by for a visit. I play poker with him from time to time and he purchased our shares of our cabin on Cordry Lake. He was excited to tell us about selling the old pontoon boat that we had and purchasing a new one. At one point his wife called and reminded him that he was late for dinner.
On Saturday my friends Rich and Kathy visited. You cannot find more loyal friends than them. They probably would’ve been there sooner but Rich had been out of town at a bowling tournament in Reno Nevada that he attends every year. He had just gotten home in the middle of the night Thursday night and he took Friday to rest up. I got to fill them in on all of the details of what had been going on even though they had been following on Facebook as well.
I also had the opportunity to talk to my sister Carol on the phone but neither she nor Karen were able to visit me. It wasn’t really necessary but it might have be nice to give dad a break. I’m sure if it had been serious they would have been there plenty.
Not much happened on Saturday or Sunday. I mostly just laid around and watched TV. Dad had decided that he could get out of our neighborhood on Sunday if he waited until the race started. Then he could hang around a little bit late and go back home after the traffic cleared. We watched the race together although he tended to sit in the chair and fall asleep quite a bit. Normally that’s not a problem when you have a DVR. If something big happens while watching a race and he missed it, I could typically just rewind and show him my own replay. No such luck in the hospital. 
Time to Leave
I slept very well Sunday night and the only bad part was I overheard some nurses talking in the hallway about Game of Thrones. I was two episodes behind and I overheard some serious spoilers. Most notably I heard about an incident with Hodor. I had successfully avoided Internet spoilers and resisted looking at articles that said “Now we know why he is called Hodor”. I thought about yelling out to them to shut up but I actually wanted to hear what they were saying. They sounded like very knowledgeable fans. 
Things naturally move slower on the weekend in the hospital and on a holiday like Memorial Day Monday I expected things to go even slower. I did get definitive word from my attending physician that I could definitely go home. I did not have my usual attending physician with the fascinating Persian accent. When the guy introduced himself I said “So you are the guy who drew the short straw and had to work on a holiday.” He said they all take turns and it comes out even in the end. I suppose I would rather work Memorial Day than Christmas or something. At least I was definitely going home. I celebrated by posting some Philip Phillips “Home” on Facebook. 
Because that pain pill had worked so well Friday night, I asked if they could write me a prescription for 6 or 8 of them so that I can have them on hand on those rare occasions when the pain returned. They had no problem doing that and I ended up getting a script for 12 of them. They were also going to change one of my medications. The Flomax that I take to help me relax my prostate so I can urinate has a warning that you should not open, crush, or chew them. That meant it could not be crushed, dissolved and put in the G-tube. They had substituted a different drug. This was all news to me because I have been chewing them for years. Well not exactly. They come in a plastic capsule which normally would have been too big for me to swallow even when I was doing pretty well swallowing. But the capsule is only about one half full of whatever powder is in there. I had always just let them soften up in my mouth, smash the outer capsule part flat, and swallowed the flattened capsule. Most of the time the contents would not spill out but even if they did, they did not taste bad. In recent months I had been actually chewing them up with no apparent ill effect.
My release orders were going to stop my diuretic bumetanide, stop the isosorbide, and switch to a different prostate medicine. I knew right away I wasn’t going to do any of that. I was going back on my regular medication and taking it orally like I had always done. But of course I did not tell them any of that. A week or so after I got home I had an appointment with my regular physician Dr. Kyrouac and he had no problem with me going back to my regular meds.
One of the things that typically delays your discharge from the hospital is the removal of catheters and IVs. I had no problem talking them into removing the catheter. That went promptly. But in the middle of the morning the nurse came in to hang another bag of antibiotic for my IV. I said “But I’m going home and they are giving me a different antibiotic for the next few days. Do we really need to do this one?” She insisted that we do. Then she dropped a bombshell on me. It was going to take 4 hours to finish.
It’s hard enough to get me dressed and get my back brace on in an unfamiliar bed. We also had the new G-tube to wrestle with. Neither dad nor I wanted to try to dress me with an IV hooked up. I have to wear an undershirt beneath my brace and the only way to get my arm through it would be to temporarily disconnect the IV and reconnect it. So we just waited an unnecessary four hours for the IV to finish.
But then it didn’t. It ended up taking an extra 45 minutes. Apparently the drip rate on the IV pump compared to the amount of fluid in a bag doesn’t always exactly finish at the appropriate time. So when it was finally over after nearly 5 hours, I thought I was ready to go and then we got another bombshell!
You just can’t stop an antibiotic IV. You have to push saline through it at the same rate that the antibiotic was going and that was going to take another hour! I was furious! One of the nurses, not the one who insisted on the IV antibiotic, asked me if I wanted to complain to a supervisor. Given my recent success with supervisory complaints I probably should have. But I didn’t want to do anything that was going to piss off the nurse who was letting me go on to do anything that would slow me down it any other way. I just thought the whole last dose of antibiotic was unnecessary and I also didn’t like the idea that 4 hours ended up being about 6.
Eventually it was all over with. Dad got me dressed and the brace went on reasonably well. After being in the hospital connected to IVs for days I had gained a lot of water weight. I’m always bloated after these things and you could tell that my brace did not close nearly as tightly as it usually does. Dad got me dressed and then nurses brought in a Hoyer lift to pick me up and put me in the wheelchair. They use a totally different kind of sling seat than the one that I use. Nobody uses the kind of seat I use. For the most part my seat is reasonably comfortable and pretty safe but one of these days I’m thinking about trying out some of the newer kinds of slings. If I need to sit on the toilet for a long time it’s a bit uncomfortable. Also I use a different seat going from the bed to my bathtub and that one isn’t quite as safe as I wish it was.
Having not set up in the wheelchair for days and having a brace on me that wasn’t in its normal position, I did not even attempt to drive myself down to the car. We had a nurse use the attendant joystick on the back of the chair to drive me. Dad drove his go-go scooter and carried everything else we had. He had already taken my laptop to the car during the four hour delay.
On the ride home my belly felt kind of weird poking through the new hole in the brace. It was a very strange feeling but fortunately it didn’t last very long. We were going to stop at the pharmacy to fill the prescription for my oral antibiotic that I would need to take for the next two or three days. I also wanted to get those pain pills just in case. I was not going to fill the Flomax substitute medication because I was going back to the Flomax. Unfortunately the Walgreens at 38th and High School Road was closed for Memorial Day. The sign in the window said there was one open at 16th and Meridian. We decided I could do without filling the prescriptions for another day. That was a decision I would later regret.
According to this post on Facebook we didn’t get home until about 5:45 Monday evening.  They had sent us home with a couple of one liter bottles of the nutritional liquid and a syringe to do the feeding. Dad’s first attempt at doing it was uneventful.
They had sent us home with a couple of one liter bottles of the nutritional liquid and a syringe to do the feeding. Dad’s first attempt at doing it was uneventful.
DVR Damage Assessment
We have two DVR’s in our home. One in the living room for things that dad and I watch together or that he watches on his own. The other one is in my bedroom and is only for stuff that I watch. I spent the rest of the evening going through both of them to see how much damage had been done by recordings overflowing in my absence. It is a proven fact that no matter how much capacity I have in a DVR, it’s never enough. Both of them are always 90-95% full. Bright House allows you to remotely schedule something to record using a webpage interface. You can also cancel a scheduled recording. Unfortunately you cannot see how much free space you currently have and you cannot see what a list of what you have recorded. I’m not talking about being able to watch your shows remotely. I just want to see what I have recorded and possibly be able to delete it remotely. You can watch many shows online especially on demand shows. But you really cannot fully manage your DVR away from home.
Sometime in the middle of the week I told dad to erase some shows from my DVR. I have a backlog of late-night shows like Jimmy Fallon and Stephen Colbert that I knew I could delete and free up some space. I would’ve liked to have seen some of those shows but missing them was no big deal. Unfortunately I did not give dad any instructions about the living room DVR. I had some old movies recorded when the IFC channel a marathon of 5 movies about time travel. I was looking for a block of time to binge watch them. They were the oldest things on the DVR but I had them protected with the “do not erase” flag set. There was a bunch of other stuff on there that was pretty old that I didn’t care if it got erased. I understood that if the machine overflowed, the oldest unprotected stuff would go first. There was enough of that that I was certain any newer shows especially dad’s shows would not be touched. I should’ve explained all that to him but I didn’t. He saw the living room DVR reach 100% so he deleted some of those old movies thinking that the old stuff was fair game. I later had explained to him my system. In some ways the older a program is, the more irreplaceable it is.
In the end the damage wasn’t too bad. A couple of the shows he deleted I was able to rerecord. A couple of those rare sci-fi time travel movies were lost but I will find them again eventually. There were actually fewer deletions that I had been expecting. The same was true in the bedroom. I lost a few things I wish I protected but there was nothing I was going to lose any sleep over.
The Pain Returns
I went to bed about 8:30 or 9 PM which is a little bit early for me but I was a bit tired after a stressful day. I watched some TV in bed but went to sleep before midnight which is early for me. I’m usually awake until maybe 1 AM or so. Dad went to sleep early as well. He was still suffering pretty badly with pain from his shingles outbreak. Unfortunately in the middle of the night my strange back pain returned. I tried some liquid Tylenol but that did not help and the pain got worse. We probably should’ve gone to the other pharmacy to get those pain pills but I only had the pain three or four times in 10 years. I didn’t really expect it to return so quickly.
Dad has some pain pills and normally I’m the strictest person you will ever find when it comes to the “don’t take other people’s prescription medicine rules.” However I was in pretty bad shape. He had two different doses available and I took one half of the smaller doses. We ground it up, dissolved it, and put it in the G-tube. That helped a little bit but not much. An hour or so later I took another half. The pain eventually went away but not as easily or as quickly as the pills that I had in the hospital and that I would eventually get filled once the pharmacy opened. 
I slept late the next day because we had been awake from 4 AM till 6:30 AM dealing with the pain. The company that was going to supply me with feeding liquid brought by a week or so worth of supplies. They told me they would also be sending a month’s worth by UPS a few days. The pain did not return Tuesday night but I did get another spell Wednesday night at about 2 AM. This time I had my own prescription and it took care of things right away. Fortunately I’ve not had any recurrence in the past three weeks. But if it ever does come back I still have plenty of those pills in reserve.
This blog is already over 13,000 words. I think will wrap this up for now. At some point I will do another blog post talking about everything that has happened since I returned home.